Nat Commun:癌细胞扩散原来也可以“传染”
2017-06-19 药明康德 学术经纬
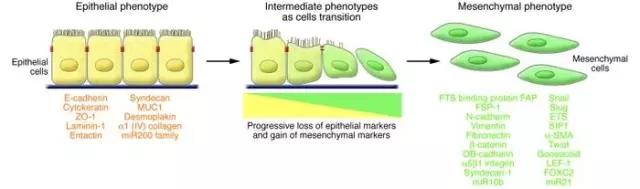
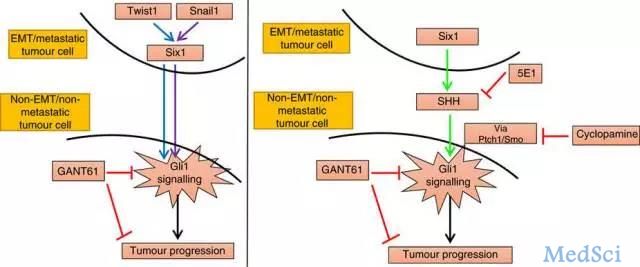
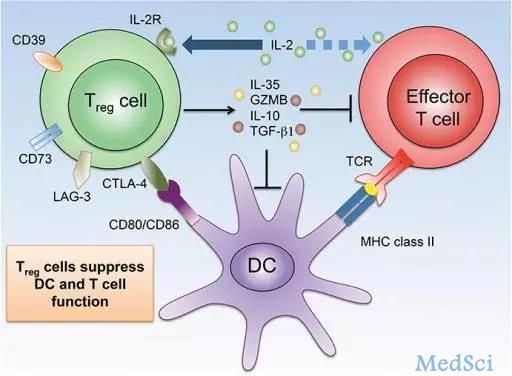
最近,科罗拉多大学(University of Colorado)的科学家在《自然》子刊《Nature Communications》上发表论文,指出转移性乳腺癌细胞可向周围正常的细胞发出信号,使得本来处于锚定状态的细胞开始扩散。这项工作揭示了癌细胞扩散相关信号通路中的重要一环,当被打断时可以降低癌症转移的可能性。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
77
#癌细胞扩散#
91
#COMMUN#
79
#癌细胞#
75
有意思。
107