免疫治疗在胰腺癌中是否有一席之地?
2017-04-15 Dr. GHL 肿瘤资讯
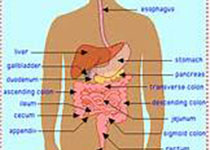
免疫治疗是肿瘤治疗中异军突起的一员,在肺癌、黑色素瘤等实体肿瘤的临床试验中都取得了很好的结果。正是因为其疗效惊人,各研究机制正努力将免疫治疗推广到更多实体瘤中。在“癌中之王”胰腺癌中,由于晚期胰腺癌的化疗药物种类十分有限,仅有吉西他滨、FOLFIRINOX(亚叶酸,5-氟尿嘧啶,伊立替康,奥沙利铂)、白蛋白紫杉醇等几种药物的疗效在临床中得到证实。因此研究者们不约而同的开始探索免疫治疗在胰腺癌中的效
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了,点个赞吧!
118
这篇文章有点拼拼凑凑嫌疑哦~
0
学习了谢谢分享!!
107
收藏
113
学习!!!!
101
巨噬细胞,骨髓来源的抑制性细胞(Myeloid-derivedsuppressorcells,MDSCs)和调节性T细胞(Treg)是早期胰腺上皮内瘤变(PanIN)阶段的三种主要白细胞亚型,主要表现为Treg数量增加、效应T细胞功能失活
70
谢谢分享,学习了
53
学习了谢谢分享。有帮助。
66
学习了很有用
58