Sci Transl Med:这款药物或能提高胰腺癌治疗效果
2017-04-11 李华芸 学术经纬
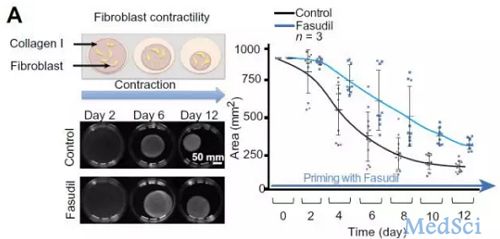
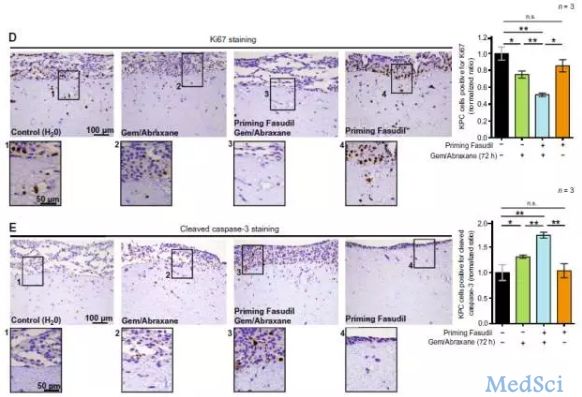
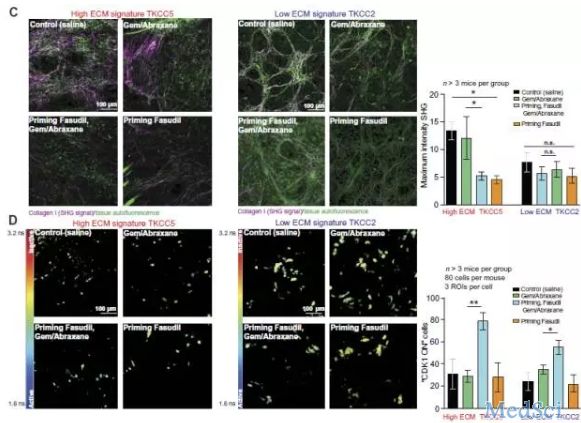
在最近一期的《科学》子刊《Science Translational Medicine》中,一项关于胰腺癌的研究登上了封面。这项重磅研究表明,一种药物能够干扰肿瘤细胞外基质的结构,从而提高化疗等标准疗法的效果。谈到胰腺癌,许多人都不会陌生。被称为“癌症之王”的它以难治而闻名,据美国癌症学会的统计,它在术后的5年生存率只有16%。多年的研究发现,胰腺癌难治的一大原因在于它表面的致密基质。它就像是一层

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗效果#
42
#Transl#
47
#TRA#
60
#Med#
39
继续关注。
63