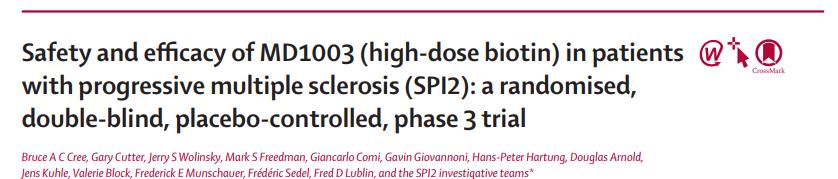
Lancet Neurol:高剂量生物素对进行性多发性硬化症患者残疾进展的影响
2020-10-27 MedSci原创 MedSci原创
高剂量、药物级生物素不能显著改善进行性多发性硬化症患者的残疾进展或步行速度,不推荐其用于进行性多发性硬化症的治疗
研究发现高剂量、药物级生物素(维生素H,MD1003)可能增强神经元和少突胶质细胞能量,改善细胞功能、修复或存活。MS-SPI研究发现,MD1003在12个月内改善了进行性多发性硬化症患者的残疾结局。近日研究人员开展SPI2研究,旨在评估MD1003在大规模临床研究中对于多发性硬化症进展型患者的安全性和有效性。
SPI2研究在13个国家的90个多发性硬化治疗中心开展。患者年龄18-65岁,诊断为原发性或继发性进行性多发性硬化症,符合修订的国际专家组标准和Lublin标准,Kurtzke功能评分值至少为2(定义为最小残疾),扩展残疾状态量表(EDSS)评分为3.5-6.5, 25英尺步行(TW25)时间低于40秒,有临床残疾进展的证据,并且在入组前2年内没有复发,随机接受MD1003(口服100毫克,每日三次)或安慰剂。研究的主要终点是12个月时EDSS或TW25与基线检查相比得到改善,以及第15个月时改善得到证实的参与者比例。
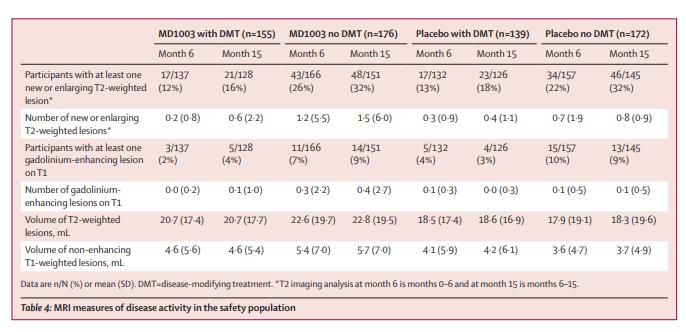
642名参与者被随机分配接受MD1003(n=326)或安慰剂(n=316)。2019年11月15日,对最后一名参与者的主要终点进行评估后,研究的双盲、安慰剂对照阶段结束,平均随访时间为20.1个月。对于主要结果,MD1003组326例患者中有39例(12%),而安慰剂组316例患者中有29例(9%)在12个月得到改善,并在15个月得到证实(优势比1.35)。MD1003组331名参与者中有277名(84%)发生了治疗-紧急不良事件,而安慰剂组的311名参与者中有264名(85%)发生了治疗-紧急不良事件。MD1003组331名参与者中有87名(26%)和安慰剂组311名参与者中有82名(26%)发生了至少一次严重的治疗-紧急不良事件。MD1003组有1例(<1%)死亡,安慰剂组无死亡。
研究认为,高剂量、药物级生物素不能显著改善进行性多发性硬化症患者的残疾进展或步行速度,不推荐其用于进行性多发性硬化症的治疗。
原始出处:
Prof Bruce A C Cree et al. Safety and efficacy of MD1003 (high-dose biotin) in patients with progressive multiple sclerosis (SPI2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. October 23, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
61
#硬化症#
60
#多发性#
55
#进行性#
66
#高剂量#
63
#Lancet#
66
#残疾进展#
75
值得学习
107
#生物素#
107
顶刊就是不一样,质量很高,内容精彩!学到很多
66