JACC:外科主动脉生物瓣失效后使用自扩张装置的TAVR
2019-05-22 xiangting MedSci原创
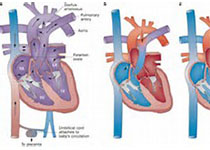
使用CoreValve或Evolut R平台进行基于导管的瓣中瓣手术可以安全地治疗退化性外科生物瓣膜。
VIVA试验(瓣中瓣)旨在系统性和前瞻性收集有关再次手术高危的外科主动脉生物瓣失效患者使用经导管主动脉瓣置换术的数据。
外科主动脉瓣置换术已成为症状性主动脉瓣病患者的标准治疗方法。然而,生物瓣膜会随着时间的推移而退化,需要重新手术。
VIVA是一项国际性、观察性、单组、上市后研究,在23个地点进行,纳入202例主动脉生物瓣膜症状性退化的患者,这些患者适合使用CoreValve或Evolut R自扩张经导管主动脉瓣进行选择性治疗。
患者为老年人(平均年龄79.9岁),47.5%为男性,平均胸外科医师协会评分为6.6%。虽然41.8%的患者有标记尺寸≤21mm的外科生物瓣膜,但瓣膜血流动力学参数从基线(平均主动脉瓣梯度35.0±16.3mmHg)到出院(17.5±8.6mmHg)有显著改善,并持续至1年(15.5±7.5mmHg)。1年时,在1.1%的患者中检测到轻度以上主动脉瓣反流。30天临床结局显示死亡率低(2.5%)、无致残性卒中、急性肾损伤率0.5%和新起搏器植入率8.0%。1年时,死亡率仍然很低(8.8%),有1例致残性卒中(0.6%)。5例患者(2.5%)出现冠脉阻塞,其中3例患者在术中出现,1例在术后即刻出现,1例在术后数月出现。
使用CoreValve或Evolut R平台进行基于导管的瓣中瓣手术可以安全地治疗退化性外科生物瓣膜。这项技术在真实世界的患者群体中达到了优异的1年临床和血液动力学结局。
原始出处:
Didier Tchétché. TAVR for Failed Surgical Aortic Bioprostheses Using a Self-Expanding Device 1-Year Results From the Prospective VIVA Postmarket Study. JACC:Cardiovascular Interventions. 27 May 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AVR#
59
#生物瓣#
76
#JACC#
48
#扩张#
58
#ACC#
52
#主动脉#
57
看了
76