Nature:科学家追踪到记忆形成新机制
2016-09-30 佚名 生物谷
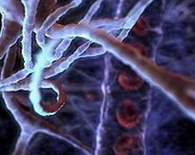
大脑通过突触的变化形成记忆。来自杜克大学等研究结构的研究人员进行了一项新研究发现了引起突触变化的意想不到的分子机制。相关研究结果发表在国际学术期刊Nature上,这些发现还对理解一些疾病如特定类型癫痫的发展带来了一些提示。在获得一段新记忆的时候,一些神经元之间的突触连接会得到加强。神经元负责接收信号的末端会变大。研究人员一直怀疑一种叫做TrkB的脑受体参与学习过程中树突棘的生长,新研究证实这个受体

大脑通过突触的变化形成记忆。来自杜克大学等研究结构的研究人员进行了一项新研究发现了引起突触变化的意想不到的分子机制。相关研究结果发表在国际学术期刊Nature上,这些发现还对理解一些疾病如特定类型癫痫的发展带来了一些提示。
在获得一段新记忆的时候,一些神经元之间的突触连接会得到加强。神经元负责接收信号的末端会变大。研究人员一直怀疑一种叫做TrkB的脑受体参与学习过程中树突棘的生长,新研究证实这个受体分子确实很重要,研究人员又进一步探索了这个受体如何发挥作用。
研究中使用了一些关键技术,其中包括一项该研究小组开发的分子传感器用来追踪TrkB的活性,他们还用显微镜对活体小鼠脑组织区域的单个树突棘进行实时观察。
研究人员利用谷氨酸作为化学信号刺激树突棘,模拟学习过程中发生的事情,发现谷氨酸能够引起树突棘的生长。而缺少了TrkB受体,树突棘在应答化学信号的时候不会生长。
由于BDNF是TrkB受体的配体分子,因此研究人员怀疑脑源性神经营养因子(BDNF)也参与其中。他们开发了一个感应BDNF的分子传感器,研究发现模拟与学习有关的信号会引起BDNF从突触后膜释放。该发现令人感到非常惊奇,因为通常认为BDNF只从负责发送信号的突触前膜释放,而非负责接收的突触后膜。
研究人员表示,虽然这些实验都以小鼠为研究模型,但是TrkB与BDNF的相互作用可能对于人的学习和记忆非常重要。
研究人员还表示在一种最常见的癫痫疾病——颞叶癫痫中也存在相同的机制。之前的工作表明TrkB受体对于颞叶癫痫的发展非常重要,在第一次发作之后短时间内抑制TrkB信号可以预防小鼠颞叶癫痫疾病的发展。
目前该研究团队正在进行更多实验进一步探索在TrkB激活之后发生的事情。除此之外,在记忆形成和癫痫发作过程中还有其他机制促进TrkB激活,研究人员也在探索其他可能机制。
原始出处
Stephen C. Harward, Nathan G. Hedrick, Charles E. Hall, Paula Parra-Bueno, Teresa A. Milner, Enhui Pan, Tal Laviv, Barbara L. Hempstead, Ryohei Yasuda, James O. McNamara.Autocrine BDNF–TrkB signalling within a single dendritic spine.Nature.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
66
真心很棒,争取早日突破,成为产品
90
真棒
78
好文章,受益颇多!
87
有意思的内容。。。
76