Science:突破!新法让癌细胞无处可逃!阻断肿瘤免疫抑制!
2018-10-29 Michael,Zoe 转化医学网
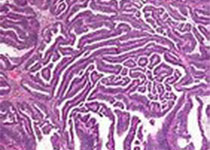
肿瘤细胞可通过许多途径逃脱免疫系统的识别和清除,其中最为出名的便是今年斩获诺贝尔医学或生理学奖的PD-1与PD-L1的相互作用。虽然抗PD-1药物已经上市,但研究人员仍在探索不同的肿瘤免疫逃避机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#阻断#
70
#癌细胞#
77
#SCIE#
117
学习了
206
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
178