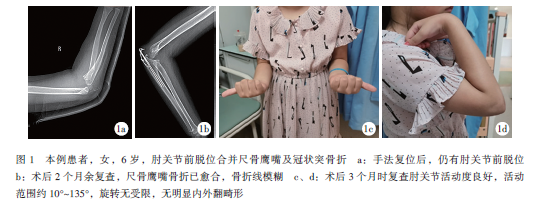
肘关节前脱位合并尺骨鹰嘴及冠状突骨折1例
2020-01-16 乔怡 王晓东 甄允方 中国矫形外科杂志
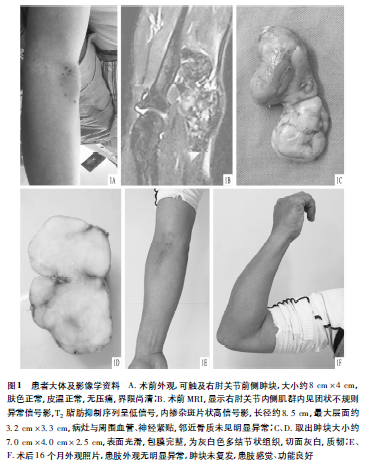
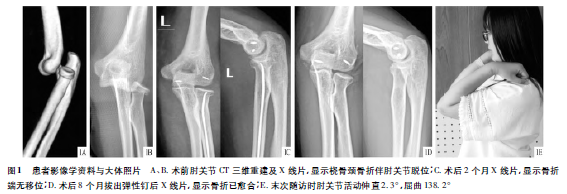
肘关节脱位在儿童并不多见,总发病率约3%,多数为后脱位,前脱位极为罕见,且多并发骨折。普通平片可明显观察到关节脱位,CT则有助于发现骨折,尤其是碎骨块嵌顿于关节内影响肘关节复位时。近期本院成功治疗一例肘关节前脱位患儿,报道如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#尺骨#
61
#肘关节#
58
#前脱位#
46
#脱位#
54