Clin Exp Otorhinolaryngol:混合性听力损失患者中耳手术后主动中耳植入术的结果研究
2021-05-03 AlexYang MedSci原创
最近,有研究人员评估了Vibrant Soundbridge(VSB)圆窗(RW)振动成形术在乳突窦切除术后持续混合性听力损失患者中的用户满意度、疗效和安全性情况。
最近,有研究人员评估了Vibrant Soundbridge(VSB)圆窗(RW)振动成形术在乳突窦切除术后持续混合性听力损失患者中的用户满意度、疗效和安全性情况。

研究包括了27名来自韩国15个三级转诊中心的乳突窦切除术后混合性听力损失患者(平均年龄58.7岁;年龄范围28-76岁;11名男性和16名女性)。VSB是在RW中植入。使用了APHAB问卷的K-IOI-HA问卷评估了用户满意度,次要结果是听力测试结果和并发症发生率。

研究结果发现,VSB手术后,APHAB调查问卷中的易于沟通(61.3% → 29.7% → 30.2%)、混响(62.1% → 43.1% → 37.4%)和背景噪音(63.3% → 37.7% → 34.3%)子量表的平均分值均明显降低。术后3个月和6个月的K-IOI-HA平均分明显高于术前的平均分(18.6 → 26.8 → 28.0)。术后VSB辅助的阈值明显低于术前未辅助和助听器(HA)辅助的阈值。术前无辅助、术前HA辅助和术后VSB助听器的最大语音平衡词识别得分之间没有明显的差异。27名患者中没有人在术后出现骨传导纯音平均值(PTA)的变化。一名患者出现暂时性面瘫,两名患者出现手术伤口感染。
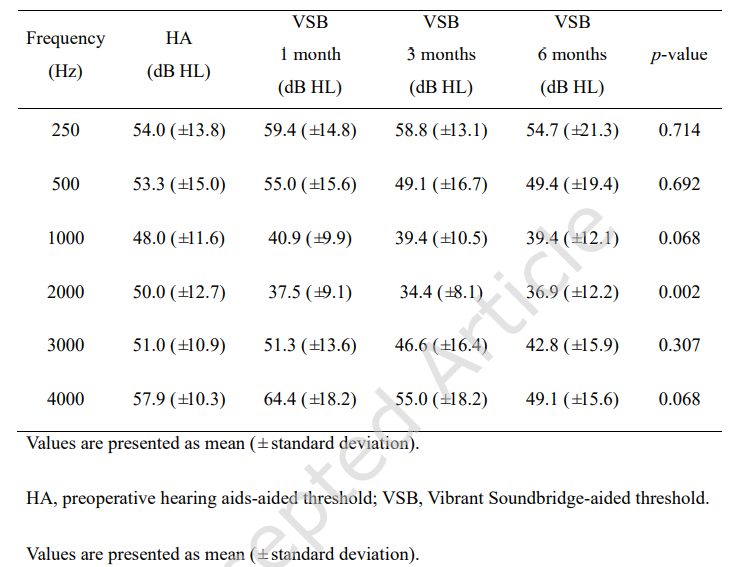
不同频率时HA辅助和VSB辅助下的阈值比较
最后,研究人员指出,RW振动成形术能使乳突窦切除术后混合性听力损失患者的满意度和听觉测试结果得到改善,并发症发生率也是可以接受的。
原始出处:
Chan Il Song , Hyong-Ho Cho , Byung Yoon Choi et al. Results of the Active Middle Ear Implantation in Patients With Mixed Hearing Loss After the Middle Ear Surgery: Prospective Multicenter Study (ROMEO Study). Clin Exp Otorhinolaryngol. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#听力#
74
#植入#
52
已读,真是受益匪浅呀!
87
术后恢复是关键
79