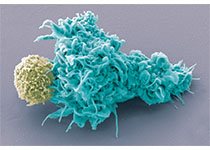
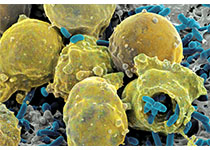
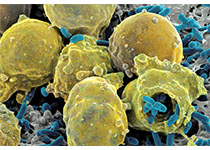
Nat Commun:科学家发现操纵癌细胞迁移扩散的“幕后黑手”!
2017-10-29 佚名 medicalxpress
癌细胞可以重新激活作为胚胎发育的重要组成部分的细胞过程。这允许他们离开原发性肿瘤,穿透周围组织并在外周器官中形成转移。在“自然通讯”杂志上,巴塞尔大学生物医学系的研究人员深入了解了调节这一过程的分子网络。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
61
#迁移#
69
#COMMUN#
82
#科学家发现#
64
#癌细胞#
77
#细胞迁移#
107
谢谢分享.阅读了.
95