腰椎间盘突出症手术方式的选择:微创还是开放?
2019-09-04 佚名 杏林之声
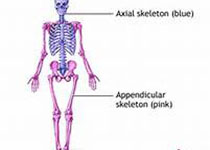
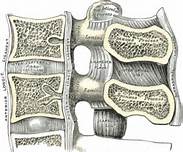
腰椎间盘突出症是较为常见的疾患之一,椎间盘相当于两个相邻椎节之间的“软垫”,在人体运动时起到缓解震荡的作用。椎间盘由外围的纤维环和中心的髓核组成。纤维环牢固地将椎体连接在一起,具有较大的弹性和坚韧性,起承受压力和防止髓核溢出的作用。髓核为白色胶状物质,富有弹性。一旦纤维环发生破裂,那么髓核就会脱离原有位置,形成突出,当突出压迫神经产生临床症状时,才称之为腰椎间盘突出症。只有椎间盘突出,没有压迫神经
引起腰椎间盘突出的主要原因是:年龄增大、长期劳累、不良生活习惯、外伤等因素作用下,椎间盘发生退变、髓核含水量降低,引起椎间高度下降、椎间小关节松动,纤维环退变、牢固程度降低,在轻微外伤诱因的进一步促进下,纤维环破裂,髓核沿纤维环破口突出,因此该疾病多发生于老年人,但现代生活节奏快,年轻人群中的发病率逐年增高。椎间盘突出,相应的椎间高度会下降,刺激窦椎神经,会导致腰痛症状;如果突出比较严重,压迫神经根,会出现坐骨神经痛症状(疼痛呈放射性,由臀部、大腿后外侧、小腿外侧至足背或足底);如果突出进一步加重或神经压迫时间过长,会导致足下垂(足趾或足踝不能背伸,行走时呈跛行步态)和马尾神经综合征(大小便功能障碍,鞍区感觉异常、性功能障碍),此时需要尽快手术治疗。
那么得了腰椎间盘突出症该怎么治疗呢?治疗可分为保守治疗和手术治疗:
保守治疗:急性发作期可选择卧床休息、牵引、对症口服或静脉注射药物等,多数病人能得到症状临时缓解。症状缓解期可继续口服药物,加强腰背肌功能练习,改变不良生活方式等加以治疗。保守治疗主要适用于:①年轻、初次发作或病程较短者;②症状较轻,休息后症状可自行缓解者;③影像学检查无明显椎管狭窄。
手术治疗:对于有以下情况之一的患者,则需要进行手术治疗:①腰腿痛症状严重,反复发作,经3个月保守治疗无效,且病情逐渐加重,影响工作和生活者;②出现马尾神经综合征或足下垂,应尽快手术治疗。
那么腰椎间盘突出症的手术方式该如何选择?手术方式可分为开放手术和微创手术。我们首先了解一下各种手术方式的优缺点。
开放手术方法又分为单纯髓核摘除术、腰椎后路减压植骨融合内固定术。30年之前,单纯髓核摘除术是治疗腰椎间盘突出症的主要术式,其方法为在腰椎的后方开个“小窗”,或者更大范围地去掉椎管后方的骨结构,这样打开椎管牵拉开神经以后就可以看到椎间盘突出的部分,在直视下直接将突出的髓核组织摘除,其优点是手术费用少,缺点是术后需要卧床休息至少8周,日后存在复发、腰椎不稳、不能缓解腰痛的可能。针对单纯髓核摘除术的缺点,后来出现了腰椎后路减压植骨融合内固定术,该术式目前是治疗腰椎间盘突出症的主流术式,该术式需要经椎弓根置入钛质螺钉,并以钛棒连接,利于对突出的椎间盘组织充分切除,彻底去除对神经组织的压迫,同时恢复椎间高度,其优点是神经减压充分、疗效可靠、不复发,能同时缓解腰痛和腿痛,术后1周即可下床活动,其缺点是手术创伤较大、费用高。
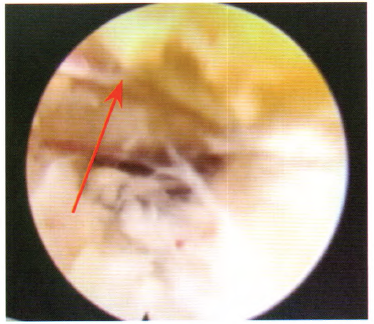
微创手术:微创手术的方法有很多种,主要包括经皮穿刺椎间盘消融术(利用臭氧、激光、化学溶解等方法使突出的椎间盘回缩)和内镜技术。前者由于疗效不可靠,已逐渐退出历史舞台,这里主要介绍内镜技术。内镜技术按入路不同,又可分为经椎间孔入路及经椎板间入路内镜微创技术,基本方法为在病人皮肤表面做一个很小的切口,将孔镜放入椎间孔或者椎板间,通过配套的手术器械将突出的突出的髓核组织摘除,达到解除神经压迫的目的。微创技术创伤小,术后恢复快,费用较低,但不是所有腰椎间盘突出症的患者都适合微创技术,微创技术有其局限性,术后不能有效缓解腰痛,术中可能不能彻底摘除突出的髓核,术后存在一定的椎间盘突出复发的可能性。腰椎间盘突出症实施内镜下微创手术一般需符合以下条件:(1)单节段腰椎间盘突出,以下肢放射痛为主要症状,而腰痛不明显;(2)突出的节段无滑脱或不稳等;(3)单纯的侧隐窝、椎间孔狭窄引起的神经根受压者。对于老年患者,一般椎间盘突出合并后方的黄韧带肥厚,椎管狭窄明显,一般也不适合内镜微创技术。
总之,对于大多数腰椎间盘突出的患者,前期都可以进行正规保守治疗,对症口服药物,避免久坐和弯腰负重,在症状缓解期加强腰背肌功能练习;只有对于出现手术适应症的患者才推荐进行手术治疗,如果出现马尾神经受损或足下垂的表现,则建议尽快手术治疗。一般情况下,对于单节段腰椎间盘突出的年青患者,以下肢放射痛为主要症状,而无明显腰痛,建议进行微创治疗,但若是存在椎管狭窄、多节段突出、合并滑脱等复杂情况的患者,则推荐进行传统手术治疗。具体的手术方案需要具体评估病情后制定出个性化的治疗方案,才能达到最好的治疗效果。
专家简介:吕碧涛,医学博士、硕士研究生导师,现为上海长征医院脊柱三科副主任医师、副教授、病区组长。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#手术方式#
61
#椎间盘突出#
43
#腰椎#
50
#微创#
58
#腰椎间盘#
68