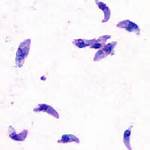
CCLM:P35和P22弓形虫抗原简短区域用于诊断妊娠期获得性弓形体病
2017-05-15 MedSci MedSci原创
P35和P22弓形虫蛋白在早期感染阶段被特异性IgG识别,使其成为急性弓形虫病妊娠控制的理想选择。研究人员已经研究了两种蛋白质以区分急性和慢性弓形虫病。然而,结果几乎不具有可比性,因为不同的蛋白质获得程序导致不同的抗原产生,所使用的参考板不具最佳代表性,并且不能进行亲合力测试或仅能勉强进行。
原始出处:
Juan G. Costa, Leandro E. Peretti, Valeria S.
García. et.al. P35 and P22 Toxoplasma gondii antigens abbreviate regions to
diagnose acquired toxoplasmosis during pregnancy: toward single-sample assays.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#获得性#
0
#妊娠期#
88
#弓形虫#
109
#抗原#
90