心脏发育机制的大发现!Science:机械应力对心脏瓣膜形成过程的调控机制
2021-11-30 苗攀登 生物探索
心脏是生命的发动机,源源不断地提供循环系统中的动力,是生物体内最关键的和最精密的器官之一。
心脏是生命的发动机,源源不断地提供循环系统中的动力,是生物体内最关键的和最精密的器官之一。在心脏内部,心房与心室之间有瓣膜,这些瓣膜使血液只能由心房流入心室而不能倒流。如此精密的结构是如何形成的呢?近日,法国国家健康与医学研究院Julien Vermot研究组在《Science》,发表了题为“Bioelectric signaling and the control of cardiac cell identity inresponse to mechanical forces”的文章,阐述了心血管瓣膜的形成过程以及机械应力在此过程中的调控机制。
机械力,如流体剪切应力和由血流和心跳产生的拉伸力,广泛存在于血液循环中。在心脏内部,心内膜细胞(EdCs)将力信号转化为细胞生化信号,诱导形成瓣膜,并且根据所属的心脏区域对力信号有不同的反应。在本研究中,以斑马鱼作为生物模型,研究了机械力调节特定的心内膜向瓣膜发育的过程。
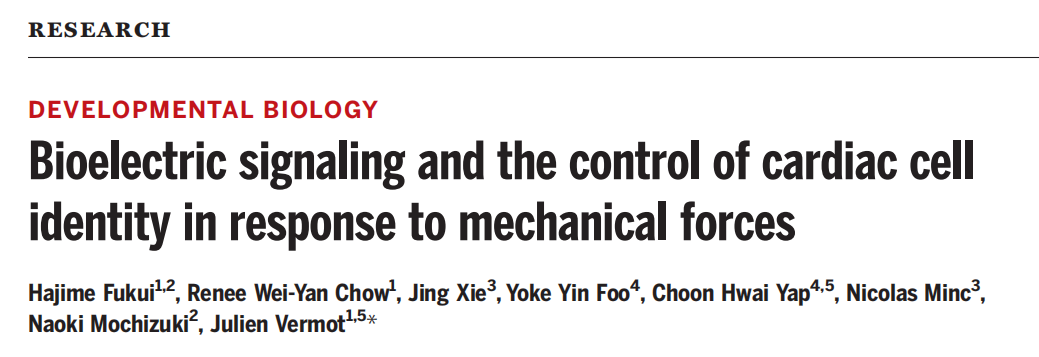
研究者们首先利用斑马鱼为生物模型对时空机械应力参数进行高精度控制,利用荧光探针(Tg)对EdCs中表达的荧光Ca2+传感器蛋白GCaMP7a进行实时成像,以监控分析心内膜细胞中的Ca2+的动态变化,结果发现Ca2+振荡几乎只会在房室瓣的房室管区域形成,因此研究者们推测,Ca2+振荡是瓣膜形成的重要因素。
Ca2+振荡几乎只会在房室瓣的房室管区域形成(上)。扫描共聚焦荧光图表征Ca2+振荡的位置(下右),胚胎受精数小时后(hpf),30-150小时内,房室管(AVC)区域的钙离子荧光峰值数目明显比心房(A, Atrium)和心室(V, Ventricle)多(下左)。
在以往的研究中已经发现,活化T细胞核因子1 (Nuclear factor of activated T cells 1, Nfatc1)是一种已知的Ca2+ 敏感的转录因子,可调节心内膜-间充质转化和心脏瓣膜形态发生。因此研究者们通过绿色荧光蛋白(GFP)荧光标记Nfatc1,来监测Ca2+信号通路。
为了确定在EdCs中观察到的Ca2+振荡是否是力响应的,研究者们利用药物(MS-222 、 p-amino)使斑马鱼停止心跳,实验结果表明,当心脏停止跳动时,EdCs中的Ca2+振荡消失,而在心跳重启后恢复。这也验证了Ca2+振荡与心内膜细胞EdCs的应力响应。
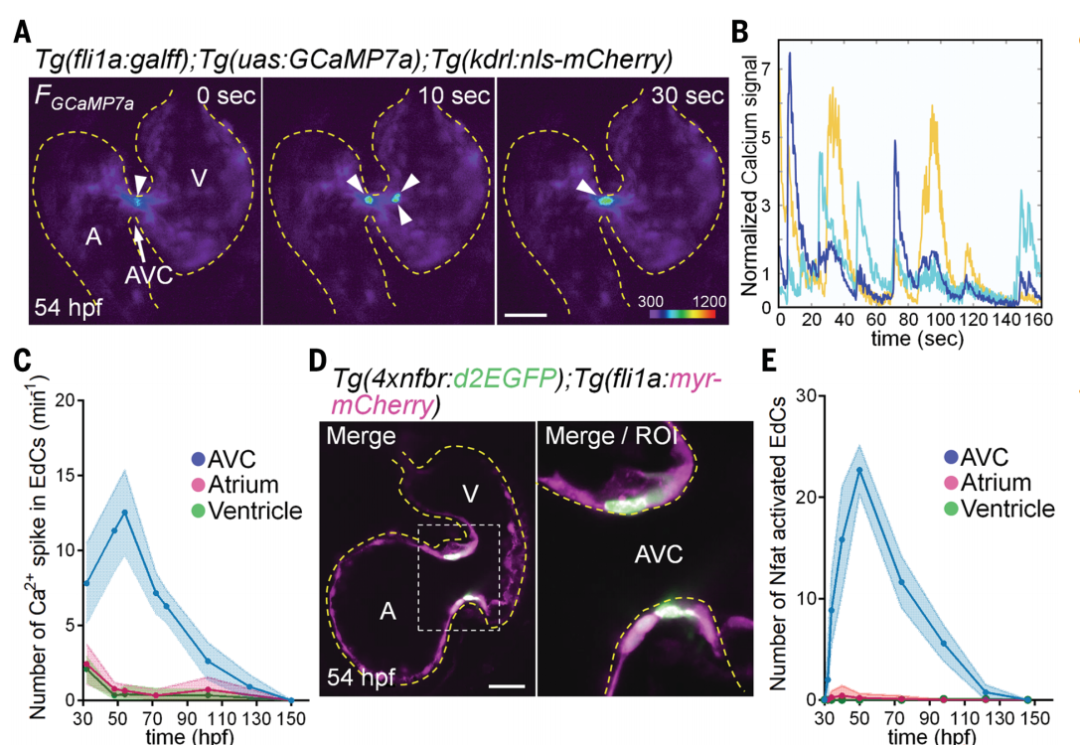
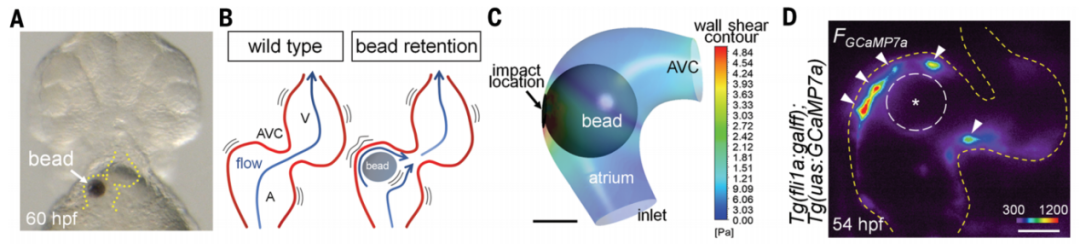
进一步地,研究者们希望通过操纵血管瓣膜边界处的机械应力对机械力改变所带来的效应进行检测。研究者们将一个30-60 μm的琼脂磁珠插入到心血管腔中,在通过磁镊操纵磁珠来改变血管瓣膜边界处的机械力,并记录Ca2+的变化。结果显示,通过外力引起的机械力的变化会导致心脏瓣膜定位异常,进一步证明了Ca2+振荡与心内膜细胞(EdCs)机械应力密切相关。
通过磁镊来操纵磁珠来改变血管瓣膜边界处的机械力。在斑马鱼房室管中插入琼脂糖磁珠(A),磁珠造成房室管处的压力异常(B、C)进而造成钙离子振荡位置异常(D)。
通过磁镊来操纵改变磁珠位置,磁珠的位置变化(F上)和钙离子振荡的位置(F下)
那么当应力发生错误的时候,是否对瓣膜形态形成和发育有影响呢?在心房内珠移植16-20小时后,在磁珠附近观察到瓣膜样的团簇。假手术空白组形成了房室管区域的瓣膜,然而,加入磁珠的实验组,心房和心室区也可见瓣膜样结构,也就是磁珠造成了瓣膜生长错乱。
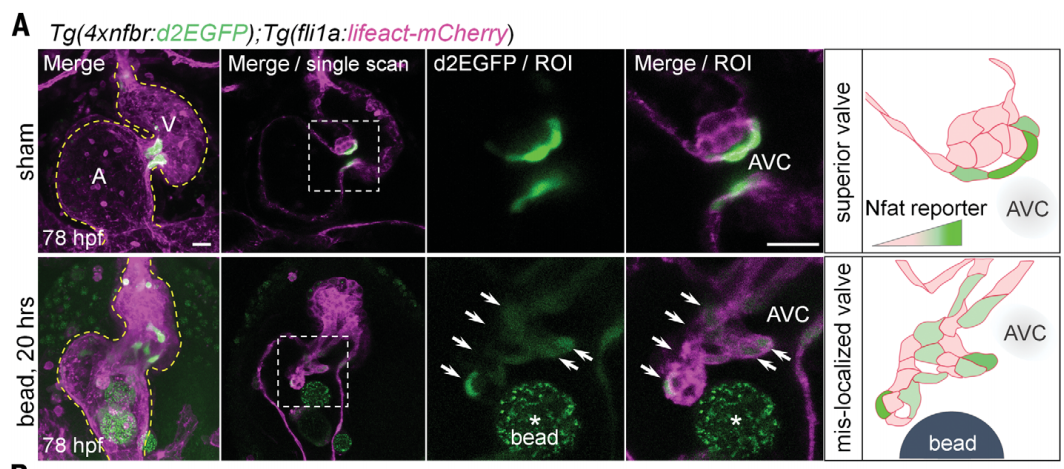
人工调控的机械力导致瓣膜位置异常
此外,研究者们还发现ATP(腺嘌呤核苷三磷酸)通过嘌呤能受体P2X通道激活Ca2+信号,使Ca2+内流。通过微注入法,将oligomycin A(清除ATP),apyrase (一种ATP水解酶), and ATPγS (ATP类似物)注入到心腔,细胞外ATP水平显著影响Ca2+显著变化。因此,P2X通道可以调节EdCs中的Ca2+内流并响应细胞外ATP水平的变化,是Nfatc1信号通路的上游,在机械力刺激下控制瓣膜发育。
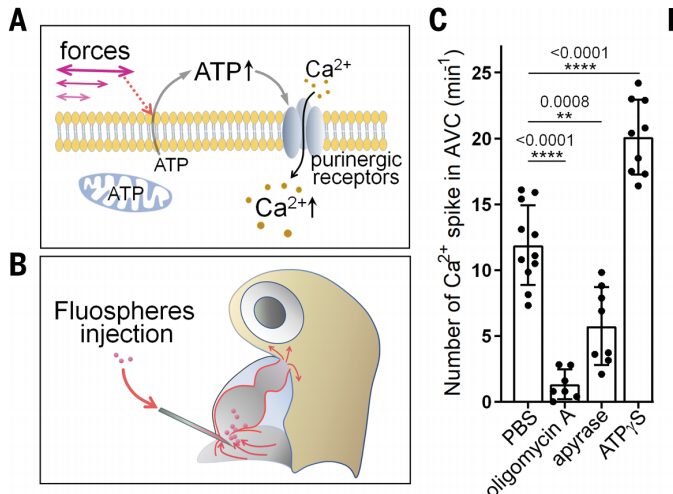
ATP调控Ca2+内流,细胞外ATP类似物可以明显增强Ca2+内流
在本研究中,研究者们确定了ATP-Ca2+是在心血管形成和瓣膜发育中形成的延伸调控通道,通过血流动力学机械力可以指导心脏瓣膜的发育。因此,ATP可以帮助心脏瓣膜在体外生长,并有可能用到先天性心脏瓣膜缺陷等疾病的治疗中。
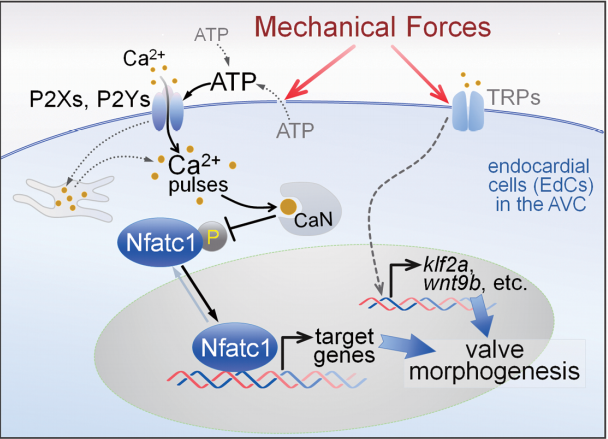
瓣膜发育的械敏感信号通路模型
总结,这项工作表明生物系统依赖于多种机械力敏感途径来精确控制形态发生过程,这也是一种保障机制,可以增强机械力调控的稳健性,避免心脏异位瓣膜形成,是生命进化的自我调控机制,也为解决相关疾病的研究提供了可靠的理论基础,在攻克心脏疾病的道路上具有非常重要的意义。
参考资料:
https://www.science.org/doi/abs/10.1126/science.abc6229
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心脏瓣膜#
41
#心脏发育#
39
#发育#
32
#SCIE#
26
#调控机制#
45
#瓣膜#
43
#应力#
47
棒
68