Ssi Transl Med:新型心脏瓣膜或可随儿童受者一起生长,减少换瓣手术次数
2021-03-19 MedSci原创 MedSci原创
如果在人类身上得到证实,这些新的心脏瓣膜可以防止每年数千名先天性心脏病患儿重复进行瓣膜置换手术。

Pixabay.com
明尼苏达大学双城分校(University of Minnesota Twin Cities)科学与工程学院(College of Science and Engineering)和医学院(Medical School)的研究人员领导的一项开创性的新研究首次表明,实验室制造的心脏瓣膜植入幼龄羔羊一年后,在受者体内能够生长。与目前使用的动物源性瓣膜相比,这种瓣膜钙化更少,血液流动功能也有所改善。
如果在人类身上得到证实,这些新的心脏瓣膜可以防止每年数千名先天性心脏病患儿重复进行瓣膜置换手术。这些瓣膜还可以保存至少6个月,这意味着它们可以为外科医生提供“现成”的治疗选择。
这项研究近日发表在美国科学促进会(AAAS)的跨学科医学期刊Science Translational Medicine上。瓣膜制造程序也已获得专利,并授权给明尼苏达大学初创公司Vascudyne,Inc.(明尼苏达州斯蒂尔沃特)。
“这是儿科心脏研究的一个巨大进步,”该研究的高级研究员、明尼苏达大学生物医学工程系和化学工程与材料科学系教授Robert Tranquillo说这是第一个将瓣膜植入大动物模型的实验,“这项研究中的例子是一只羔羊,植入的瓣膜可以随着动物成长到成年。我们还有一段路要走,但这使我们在未来儿童临床试验的道路上走得更远。我们对未来几年这一现实的可能性感到兴奋和乐观。”
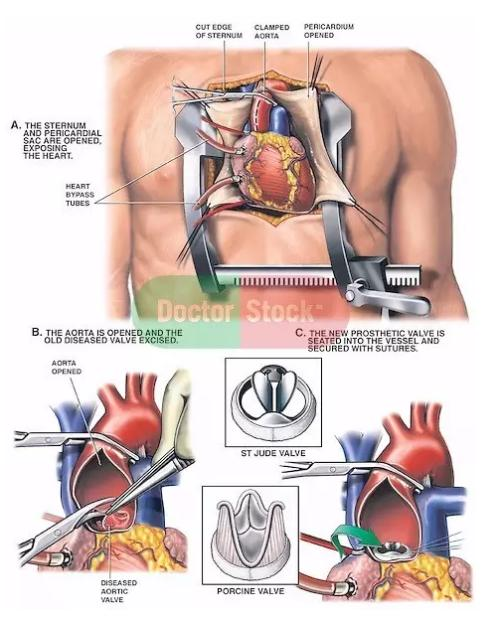
目前,研究人员还没有能够开发出一种能够为儿童患者生长和维持功能的心脏瓣膜。对于这些患有心脏缺陷的儿童来说,唯一可接受的选择是由经过化学处理的动物组织制成的瓣膜,这些组织常常因钙化而功能失调,需要更换,因为它们不能随儿童生长。这些孩子通常需要忍受多达五次(或更多)的心脏直视手术,直到成年后植入机械瓣膜。这就要求他们终生服用血液稀释剂。
在这项研究中,Tranquillo和他的同事使用了组织工程和再生医学的混合体来制造生长中的心脏瓣膜。在八周的时间里,他们使用了一种专门的组织工程技术,在实验室里从一个产后捐赠者的皮肤细胞中产生了血管样的管子。为了研制这种试管,研究人员将供体羊皮细胞与一种类似明胶的物质(称为纤维蛋白)以试管的形式结合起来,然后利用生物反应器提供细胞生长所需的营养物质。
然后,研究人员用特殊的清洁剂将羊细胞从类似组织的试管中洗掉,留下一种无细胞的胶原基质,植入后不会引起免疫反应。这意味着这些试管可以储存和植入,而无需使用受体细胞进行定制生长。
下一步是将其中三根管子(直径约16毫米)精确地缝在一起,形成一个封闭的环。然后,研究人员将它们稍微修剪一下,制造出小叶,复制出一个直径约19毫米的类似心脏瓣膜的结构。
“经过这些最初的步骤,它看起来像一个心脏瓣膜,但问题是它是否可以像心脏瓣膜一样工作,是否可以生长,”Tranquillo说这项研究发现证实了这两个点。
将第二代三管瓣膜植入三只羔羊的肺动脉。52周后,瓣膜再生,因为其基质被来自受体羔羊的细胞填充,并且直径从19mm增加到生理正常的瓣膜约25mm。研究人员还发现,根据超声波图像测量,瓣膜小叶的长度增加了17%到34%。此外,研究人员还表明,三管瓣膜比目前的动物源性瓣膜工作得更好,几乎没有其他瓣膜植入同龄羔羊后出现的钙化或凝血现象。
Zeeshan Syedain说:“我们从以前的研究中知道,工程管有能力在生长中的羔羊模型中再生和生长,但最大的挑战是如何在一年内经历4000万个循环的生长中维持小叶功能。”,这项研究的首席研究员,同时也是明尼苏达大学的高级研究员,在Tranquillo的实验室里,“我们看到从小羊到成年羊的整个一年中,瓣膜的功能都很好,这是非常令人兴奋的。”
接下来的步骤是将三管瓣膜直接植入心脏右心室,模拟最常见的外科修复,然后开始申请美国食品和药物管理局(FDA)批准在未来几年进行人体临床试验。
“如果有一天我们能让这些儿童瓣膜获得批准,这将对患有心脏缺陷的儿童和他们的家庭产生巨大的影响,因为他们不得不面对多次手术带来的巨大压力,”Tranquillo说,“我们有可能把这些孩子必须忍受的手术次数从五次减少到一次。这就是梦想。”
参考文献:Zeeshan H. Syedain, Bee Haynie, Sandra L. Johnson, Matthew Lahti, James Berry, John P. Carney, Jirong Li, Ryan C. Hill, Kirk C. Hansen, Greeshma Thrivikraman, Richard Bianco, Robert T. Tranquillo. Pediatric tri-tube valved conduits made from fibroblast-produced extracellular matrix evaluated over 52 weeks in growing lambs. Science Translational Medicine, 2021; 13 (585): eabb7225 DOI: 10.1126/scitranslmed.abb7225
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TRA#
48
#Transl#
47
#SSI#
84
#心脏瓣膜#
56
但愿如此啊!
0
#瓣膜#
63
#Med#
54
学习了谢谢
99