Leuk Lymphoma:CD19 CAR T疗法可用于治疗存在T315I突变的复发性Ph+ALL患者
2021-05-01 MedSci原创 MedSci原创
目前,对存在T315I突变的复发性Ph+ALL的有效治疗方法不多;CD19 CAR T是治疗此类患者的潜在疗法。近日,研究人员报告了CD19 CAR T疗法治疗7例具有T315I突变的复发性Ph+AL
目前,对存在T315I突变的复发性Ph+ALL的有效治疗方法不多;CD19 CAR T是治疗此类患者的潜在疗法。近日,研究人员报告了CD19 CAR T疗法治疗7例具有T315I突变的复发性Ph+ALL患者的研究结果,研究已发表于Leuk Lymphoma。

这7例具有T315I突变的复发性Ph+ALL患者在allo-HSCT前或后接受了CD19特异性CAR T细胞治疗。
结果显示,在这7名病例中,有6名在第一次输注CAR T细胞后1个月内进入CR或CRp。6名患者的MRD快速下降。4/5例患者的BCR/ABL融合转录物为阴性(2例未进行)。直到最后一次随访,3名患者保持缓解,但是没有通过QPCR检测MRD来证实,其中2名患者同时接受了抗CD19 CAR T细胞和普纳替尼。
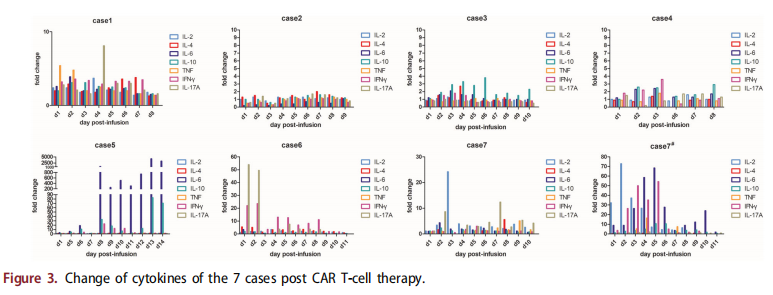
综上所述,该研究结果证实了抗CD19 CAR T细胞疗法在治疗allo-HSCT前后T315I突变的复发性Ph+ALL中的疗效,以及该疗法可与普纳替尼联合使用。
原始出处:
Fei Yang, et al., Anti-CD19 chimeric antigen receptor T-cells induce durable remission in relapsed Philadelphia chromosome-positive ALL with T315I mutation. Leuk Lymphoma. 2020 Feb;61(2):429-436. doi: 10.1080/10428194.2019.1663417.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发性#
58
#lymphoma#
71
#ALL#
71
#CD19#
92
学习了,谢谢分享
101
学习了,涨知识了!
93
👍
85