J Thromb Haemost:血小板来源的微泡水平与静脉血栓栓塞风险相关
2022-01-21 MedSci原创 MedSci原创
该研究的结果表明,较高比例的PD微泡与未来发生VTE的风险相关,并提示血小板活化在VTE发病机制中的作用。
微泡是从细胞中脱落出来的较小的双膜封装颗粒。病例对照研究报道了静脉血栓栓塞(VTE)患者血浆中血小板来源的微泡(PD微泡)水平升高。然而,目前尚不清楚较高的PD微泡水平是否是急性VTE事件的危险因素或结局。
近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,该研究旨在明确血浆中PD微泡与未来发生VTE的风险之间的关联。

研究人员对314例VTE病例和705例年龄和性别匹配的对照者(来自Tromsø研究)进行了一项基于人群的嵌套病例对照研究,研究人员分析了血浆中PD微泡的比例(%)与未来静脉血栓栓塞事件风险之间的关联。研究人员从基线(即VTE发生之前)取样的血浆中分离出的微泡染上血小板标志物并通过流式细胞术进行分析。PD微泡的比例定义为PD微泡数量除以微泡的总数。研究人员根据PD微泡的比例不同四分位数估计了VTE风险的比值比(ORs)与95%置信区间(CI)。
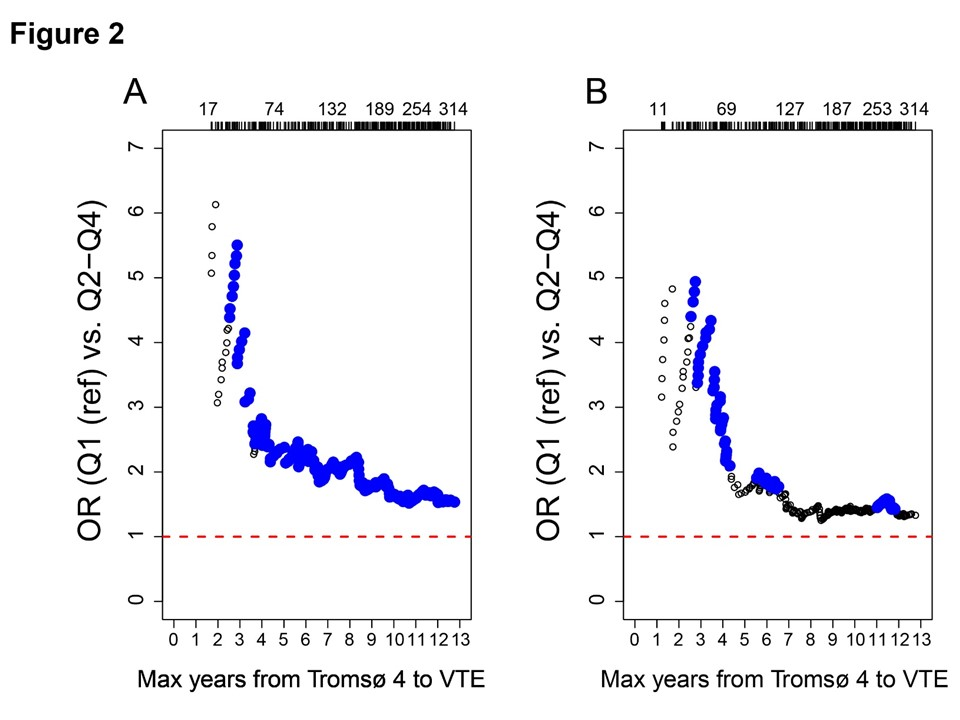
与PD微泡的比例为最低四分位数的受试者相比,PD微泡的比例最高四分位数的受试者发生VTE的OR为1.78(95%CI为1.21-2.64),诱发的VTE为1.99(95%CI为1.24-3.26)。研究人员对年龄、性别、BMI、CRP、血小板计数和癌症进行了多变量调整后,该关联受到了中度程度的影响。当采血和VTE事件之间的时间较短时,VTE的OR较高。
由此可见,该研究的结果表明,较高比例的PD微泡与未来发生VTE的风险相关,并提示血小板活化在VTE发病机制中的作用。
原始出处:
Omri Snir.et al.Plasma levels of platelet-derived microvesicles are associated with risk of future venous thromboembolism.Journal of Thrombosis and Haemostasis.2022.https://onlinelibrary.wiley.com/doi/10.1111/jth.15638?af=R
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#静脉#
61
#静脉血#
105
#HAE#
52
#静脉血栓栓塞风险#
92
#微泡#
67