CHMP对 Kineret (anakinra) 治疗COVID-19持积极意见
2021-12-19 Allan MedSci原创
欧洲药品管理局已向欧盟委员会建议批准在 COVID-19 中使用 Kineret (anakinra),该委员会将发布最终决定。
欧洲药品管理局已向欧盟委员会建议批准在 COVID-19 中使用 Kineret (anakinra),该委员会将发布最终决定。
欧洲药品管理局人用药品委员会 (CHMP) 对 Kineret (anakinra) 持积极意见。Kineret (anakinra) 是一种治疗成人肺炎患者冠状病毒病的药物。该药物由瑞典公司 Biovitrum AB (Sobi) 开发,适用于需要补充氧气(低流量或高流量氧气)且有发展为严重呼吸衰竭疾病的患者。
由于感染者的炎症反应过度反应(通常称为“细胞因子风暴”),COVID-19 感染可导致死亡。 Anakinra 是一种抗炎疗法,通过靶向细胞因子 IL-1α/β 起作用,IL-1α/β 有助于 COVID-19 诱导的过度炎症。因此,阻断这种细胞因子可以对 COVID-19 疾病进展产生重要影响。
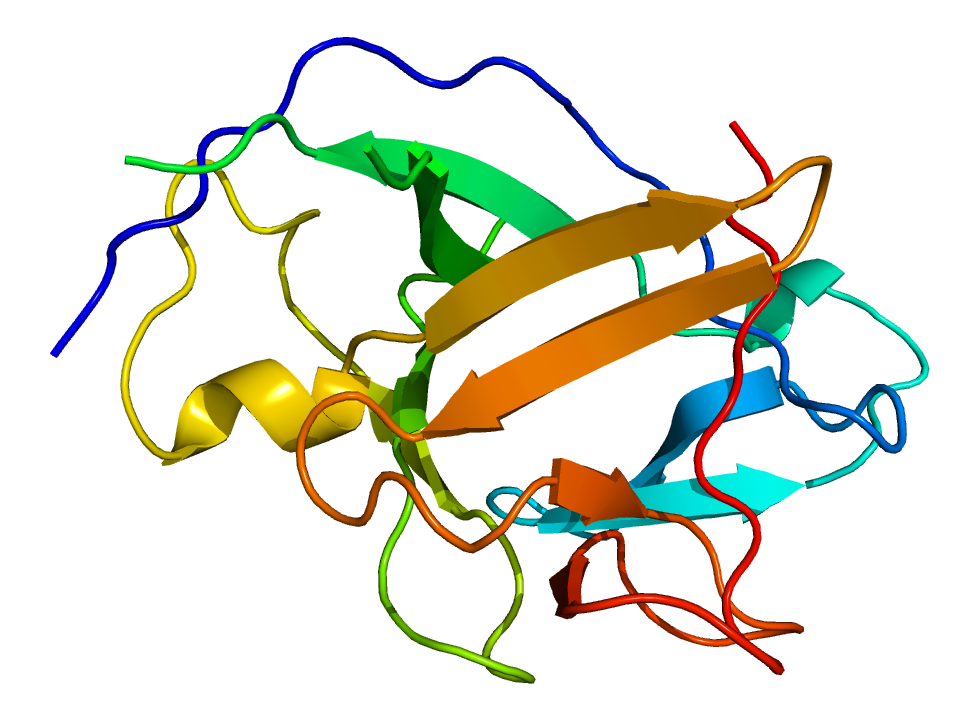
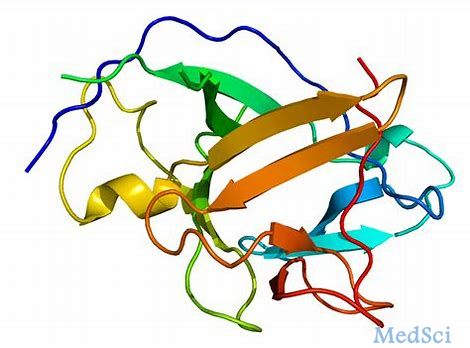
图.IL-1的三维结构
CHMP 的积极意见是基于 SAVE-MORE III 期临床研究的结果,该研究发现,早期识别具有可溶性尿激酶纤溶酶原激活剂受体 (suPAR) 的候选患者,然后用anakinra治疗,将减少64%进展为严重疾病和死亡的患者。该研究还发现死亡率相对下降了55%,细胞因子风暴患者的死亡率相对下降了80%。
SAVE-MORE 研究利用以前试验的经验,证明了anakinra对尚未进展为严重呼吸衰竭但预后较差的患者的疗效。这是由炎症的血浆生物标志物所鉴定的。
Sobi 研发主管兼首席医疗官 Ravi Rao 说:“在许多国家在继续照顾重病患者时仍面临巨大压力的时候,今天 CHMP 的积极意见代表了治疗 COVID-19 的一个重要里程碑。如果获得欧盟委员会的批准,这对欧洲许多人来说将是个好消息”。
先前,KINERET (anakinra) 被欧盟批准用于治疗中重度活动性类风湿性关节炎、Cryopyrin 相关周期性综合征 (CAPS)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ANA#
81
#INR#
76
#RET#
94
#CHMP#
138
#AKI#
82
#anakinra#
79