没有人没抽过筋吧?
那种晚上抽筋抽醒的经历
是人都不会想再经历一次了……
大晚上汗流浃背
呼吸变快
咬牙切齿叫出声
等待抽筋缓过去的时间
一秒万年
前几天有个同学问了腿抽筋的问题
今天就来讲讲嗷!
抽筋是缺钙了吗?
还有别的原因!
我们说到脚抽筋,只会想到“缺钙”,但真相总是不止一个……
知道腿抽筋的原因,可以帮助大家更好地预防它!而且腿抽筋如果让其发展下去,是很有可能造成疾病变得严重的!
原因一、寒冷刺激
咱们的身体,受到寒冷刺激的,骨骼肌就会发生不自主的抽搐——这是机体为了产生更多的热量,用以保护重要的内脏而迫不得已的行为。因为如果身体温度过低,容易引起功能性障碍,甚至危及生命。
·原因二、劳累、肌肉短时间内伸缩过快
把肌肉弄累了,它们也是会“反抗”的!过度运动,短时间内因为肌肉收缩或者舒张过快,容易导致肌肉在短时间内进行无氧呼吸,乳酸的积累会让刺激肌肉之间的协调性,在收缩的同时强制性舒张。
冲突产生了,抽搐也就来了。
·原因三、缺钙/缺镁
钙离子是肌束收缩必要的媒介,少了钙离子,那么肌肉不但会感觉到肌肉收缩力度降低,而且还会导致抽搐。这样的情况比较容易发生在小孩子,孕妇老人等人群身上。
同时,缺镁的情况下也会导致肌肉痉挛。镁离子是细胞内的重要物质,如果血液中镁不足,会导致细胞内钾离子外泄,神经肌肉因细胞内钾不足而兴奋增强,出现肌肉痉挛的现象。
·原因四、中枢神经系统发生问题
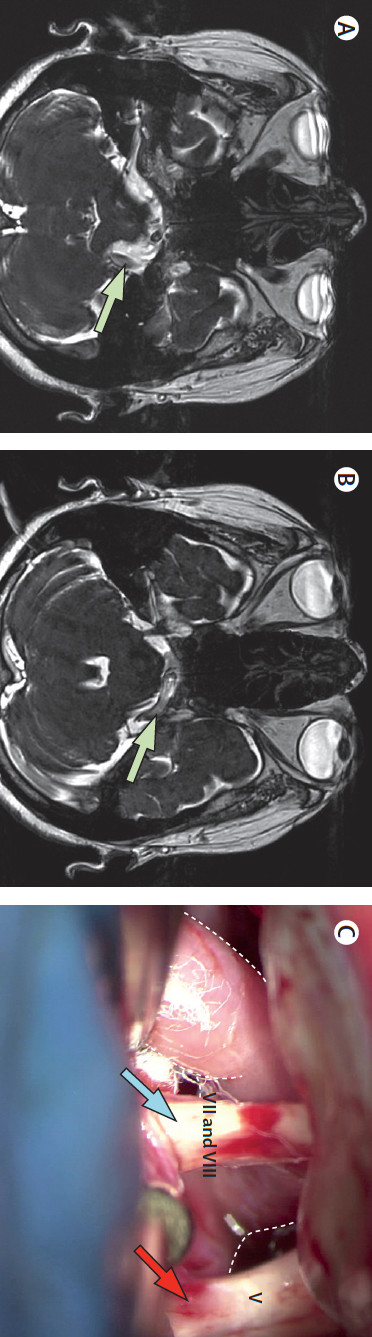
肌肉都是受到神经系统的支配,因此如果中枢神经系统发生了问题,特别是下行的神经元,出现了问题很容易导致肌肉抽搐,例如癫痫,因此如果家族里面有过癫痫发作的患者,那么自己也应该十分重视。
肌肉抽筋不可怕,
这些技巧帮你忙
在平时我们做强烈运动的时候,就应该先热身,一者让肌肉得到适应,二来韧带这些也是得到充分的拉伸。
同时,晚上腿部的保暖工作也要做好,特别是在劳累之后更要注意一些。
当然啦充足的营养也是十分重要的,不过我们在补钙的时候也又很多误区,钙补充的时候应该同时补充维生素D,这样可以促进钙质的吸收。
那抽筋之后咋整呢?
发生肌肉抽搐的时候,你需要一些勇气,冷静下来。轻度的抽搐只需要让肢体往收缩方向相反的位置拉伸,比如用手扳住前脚掌,拉伸小腿肌肉,坚持一段时间,便可缓解~
但是!如果是反复发生,而且程度越来越严重的抽搐就需要及时看医生啦!
你们还有啥问题吗!!!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













的确是这样
66
的确
73
的确
77
学习学习
87
#睡觉#
92