Cell Metab:意外!肥胖易增加糖尿病风险,背后有个关键分子
2018-10-17 悠然 生物探索
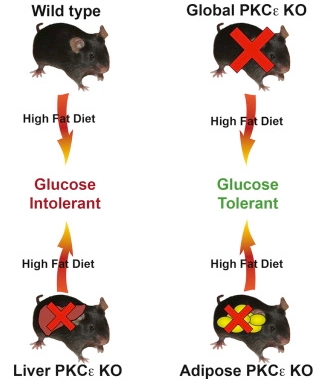
10月11日,《Cell Metabolism》期刊新发表了这一篇题为“Protein Kinase C Epsilon Deletion in Adipose Tissue, but Not in Liver, Improves Glucose Tolerance”的文章,揭示了一种关键酶——蛋白激酶C ε(protein kinase C epsilon,PKCε)在糖尿病中的代谢细节。这一研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CEL#
79
#Cell#
60
#MET#
58
#Meta#
71
学习了谢谢
99
谢谢MedSci提供最新的资讯
88