Cancer Cell:癌细胞可以高效代谢果糖——急性髓细胞白血病研究的新发现
2016-10-16 佚名 麦特绘谱
上海交大附属第六人民医院转化医学中心贾伟教授课题组在与上海血液学研究所陈赛娟教授课题组的合作研究中发现,急性髓细胞白血病(AML)细胞具有极强的果糖代谢能力,而活跃的果糖代谢促进白血病的恶性进展。这项研究于2016年10月13日在线发表于癌症研究领域顶级学术期刊Cancer Cell杂志(链接为:http://www.cell.com/cancer-cell/fulltext/S1535- 610
上海交大附属第六人民医院转化医学中心贾伟教授课题组在与上海血液学研究所陈赛娟教授课题组的合作研究中发现,急性髓细胞白血病(AML)细胞具有极强的果糖代谢能力,而活跃的果糖代谢促进白血病的恶性进展。这项研究于2016年10月13日在线发表于癌症研究领域顶级学术期刊Cancer Cell杂志(链接为:http://www.cell.com/cancer-cell/fulltext/S1535- 6108(16)30441-X),研究论文的题目是“Enhanced fructose utilization mediated by SLC2A5 is a unique metabolic feature of acute myeloid leukemia with therapeutic potential”。贾伟教授和陈赛娟教授是这篇论文的共同通讯作者。陈文连博士、王月英博士和赵爱华博士为共同第一作者。
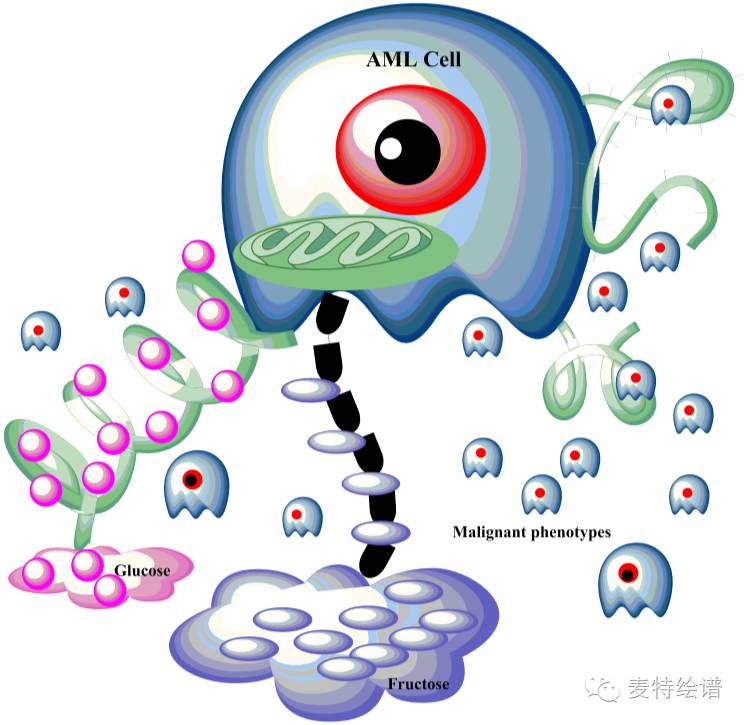
上述两个课题组合作,于2014年在国际学术期刊BLOOD(《血液》杂志)上发表了急性髓细胞白血病代谢组学的研究工作。研究发现AML患者整体代谢谱出现显著变化,通过自上而下(Top-down approach)的系统生物学研究思路,研究团队发现AML患者的糖酵解代谢水平非常活跃,而且患者的糖酵解代谢活性越高,其生存就越差。研究团队还发现,活跃的糖酵解代谢可显著降低AML细胞对化疗药阿糖胞苷的敏感性。研究人员在后续的工作中观察到,AML细胞异常活跃的糖酵解代谢可导致骨髓微环境中葡萄糖水平严重不足,而这种情况下AML细胞如何保持足量的碳源摄取以维持细胞的恶性增殖可能是一个十分重要的癌症代谢新机制。随着研究的进一步深入,他们获得了一个重要发现:在葡萄糖缺乏的情况下,AML细胞可启动一个替代机制转而利用果糖。果糖是人体血液系统中的第二大血糖,它的细胞转运由SLC2A5基因编码的GLUT5蛋白转运子介导。
研究团队发现,AML细胞表达的SLC2A5基因水平越高(即利用果糖的能力越强),则患者的预后越差。使用RNA沉默技术干扰AML细胞的SLC2A5基因表达,可显著降低细胞对果糖的摄取以及果糖诱导的细胞增殖。
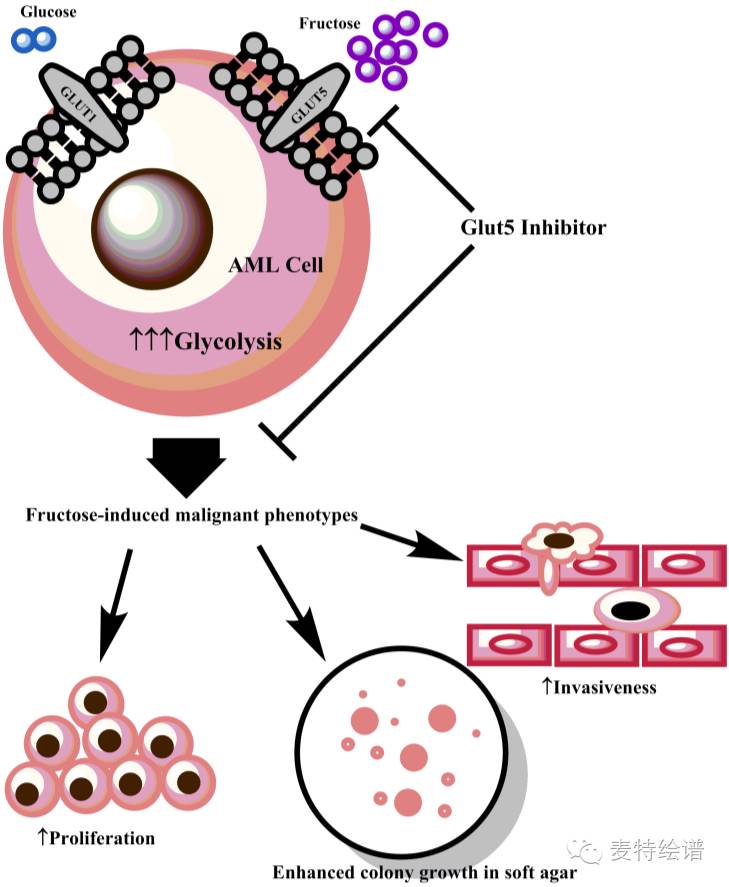
在此发现的基础上,研究团队使用了一个小分子药物来特异性地阻断果糖的跨膜转运,这个抑制果糖利用的措施可以在体外细胞模型中显著抑制细胞的恶性增殖和浸润。而在AML动物模型中,使用该小分子药物阻断果糖的AML细胞跨膜转运可显著改善小鼠的白血病症状并延长小鼠的生存。值得关注的是,该小分子药物可与化疗药阿糖胞苷协同作用,进一步改善治疗效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新发现#
74
#髓细胞白血病#
79
#CEL#
122
#cancer cell#
78
#Cell#
70
继续关注
146
继续学习
117
继续关注
107
继续学习
96
#癌细胞#
114