Gastric Cancer:术后C反应蛋白升高与并发症发生的相关关系
2020-08-08 MedSci原创 MedSci原创
胃癌是全世界常见的恶性肿瘤,虽然手术切除是最有效的根治性治疗,许多患者仍出现胃癌的复发。
胃癌是全世界常见的恶性肿瘤,虽然手术切除是最有效的根治性治疗,许多患者仍出现胃癌的复发。病理性TNM分期是手术后预后的最有用指标,但是仍有不足,因此,我们需要额外的预后指标来补充可切除胃癌患者的TNM分期并确定最佳的术后策略。已经有研究已经表明,术后并发症的发生会增加炎性细胞因子的水平,例如白细胞介素-6(IL-6),并且可以导致残留的癌细胞增殖。
C-反应蛋白(CRP)是全身性炎症的最常见的生物学指标,与血清IL-6水平密切相关。因此,研究人员进行了这项多中心验证研究,以确认1400例接受了pT2-T4胃癌手术切除的患者的术后CRP升高的预后价值。

研究人员从21个医疗机构中收集了1456例接受切除手术的pT2-T4胃癌患者的数据。使用Kaplan–Meier方法评估住院期间术后CRP最高血清水平(CRP max)的预后价值。CRP max的预后独立性通过无复发生存期(CRS)的Cox多变量分析进行评估。
研究结果显示:高CRP max(≥12 mg / dL)组的RFS 显着低于低CRP max(<12 mg / dL)组的无复发生存期(RFS)(P= 0.002)。复发模型显示,高CRP max组(9.2%)比低CRP max组(4.7%)发生肝转移的频率更高(P= 0.001)。在没有腹腔内感染并发症的患者中,高CRP max组的RFS明显低于低CRP max组(P= 0.026)。在腹腔内感染并发症患者中,高CRP max组的RFS较低CRP max组低组,但这种差异不明显(P = 0.075)。用13个协变量进行Cox多变量分析表明,CRP max(P= 0.043)是独立的预后因素。
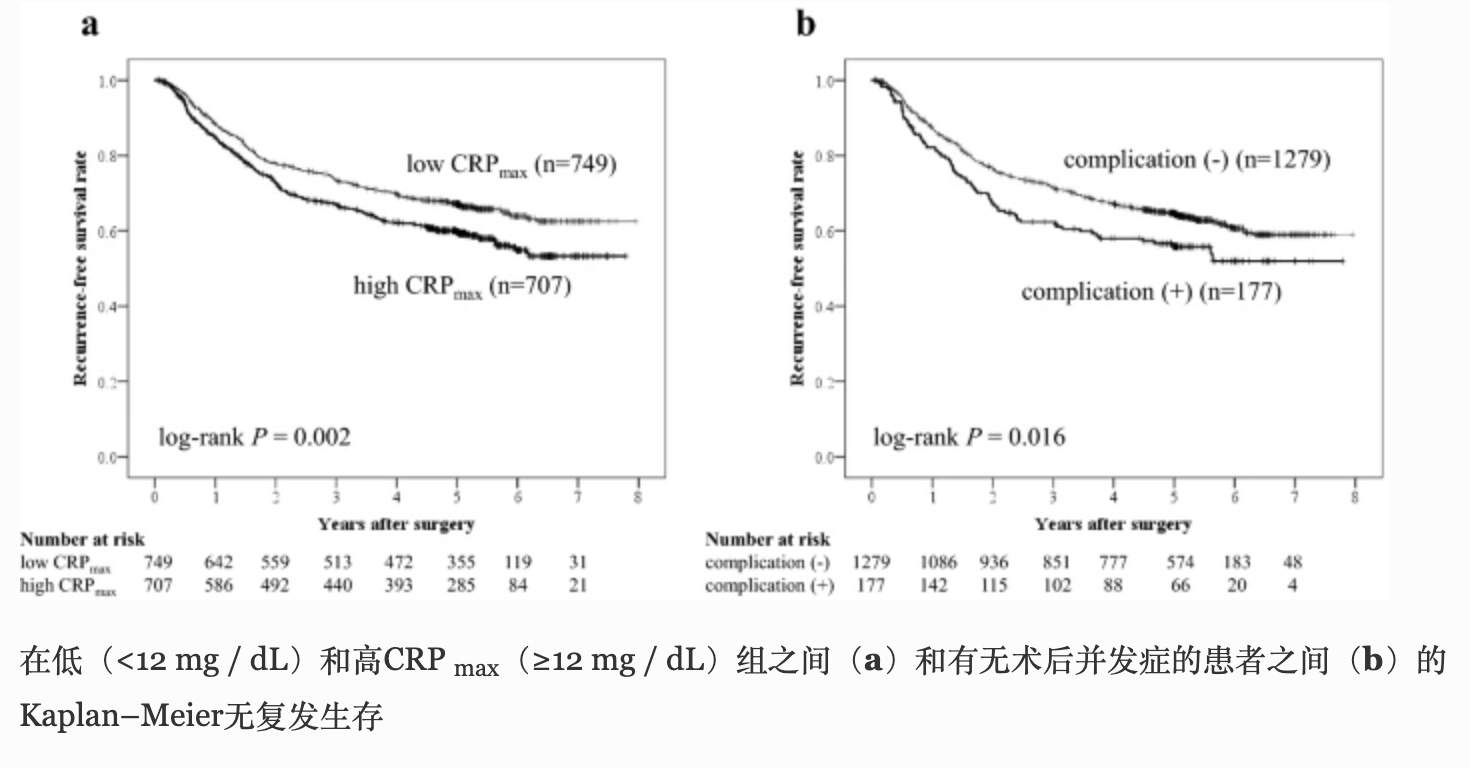
本项研究证实与腹腔内感染并发症的发生相比,术后CRP升高是胃癌患者预后的更好预测指标。
原始出处:
Yukinori Kurokawa. Et al. Prognostic value of postoperative C-reactive protein elevation versus complication occurrence: a multicenter validation study. Gastric Cancer.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#并发#
81
#GAS#
74
#相关关系#
80
受益匪浅
93
#gastric#
0
#AST#
66
#C反应蛋白#
79
学习了
129