研究发现肿瘤微环境导致获得性耐药新机制
2016-01-22 黄辛 中国科学报
中科院上海健康所 研究发现肿瘤微环境导致获得性耐药新机制 中科院上海生科院上海交大医学院健康科学研究所孙宇研究组揭示了Wnt信号通路在肿瘤耐药性形成过程中的核心地位和分子机制,颠覆了人们对于SFRP2分子在很多癌型中对于Wnt通路拮抗作用的传统认识。相关成果近日在线发表于《癌基因》 。 研究人员以全基因组表达谱分析发现,一种与Wnt信号通路调控有关的可溶因子SFRP2在经过基因毒试剂处理
中科院上海健康所 研究发现肿瘤微环境导致获得性耐药新机制
中科院上海生科院上海交大医学院健康科学研究所孙宇研究组揭示了Wnt信号通路在肿瘤耐药性形成过程中的核心地位和分子机制,颠覆了人们对于SFRP2分子在很多癌型中对于Wnt通路拮抗作用的传统认识。相关成果近日在线发表于《癌基因》 。
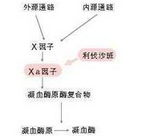
研究人员以全基因组表达谱分析发现,一种与Wnt信号通路调控有关的可溶因子SFRP2在经过基因毒试剂处理过的前列腺基质细胞PSC27中被高度上调。癌细胞的增殖率、迁移率、侵袭性和异质性,均在广谱PSC27-RAD胞外液作用下大幅提高,而一旦SFRP2被清除,以上活性则显著减弱。WNT16B上调前列腺癌细胞对化疗试剂的耐受性,而SFRP2的存在却使其更加明显,暗示前者是该过程的中心分子、后者为辅助因素。利用促使前列腺癌组织内细胞凋亡程度显著上升的WNT16B特异性抗体,模拟临床治疗条件下的生理现实,针对负荷移植瘤的免疫缺陷型小鼠进行化疗和抗体给药,发现化疗本身使得肿瘤减小近40%,而协同使用免疫疗法可以进一步缩小肿块。
该研究发现微环境中的SFRP2实际是Wnt通路兴奋剂,而特异性抑制WNT16B可促进体内条件下肿瘤细胞凋亡,剥夺肿瘤从损伤性激活的微环境获得耐药性的途径,降低肿瘤对化疗药物的耐药性,为将来转化医学提供了重要借鉴和实验依据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#获得性#
90
#研究发现#
70
#获得性耐药#
87
学习了 继续关注
143
不错,赞一个
137
这篇文章有一定深度
123
是一篇不错的文章
119
非常实用
164
值得进一步关注
171
文章有深度
118