产前超声诊断脊髓纵裂畸形1例
2019-01-21 刘志兴 陈莉 袁新春 中国超声医学杂志
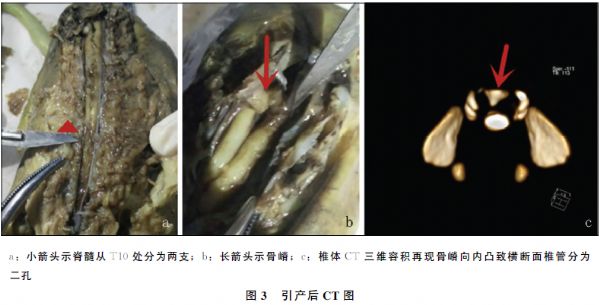
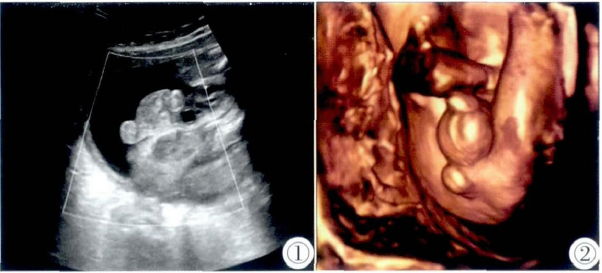
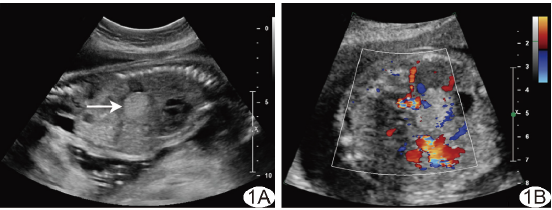
孕妇,20岁。孕1产0,孕22+3周,孕期无服用药物及毒物接触史,因常规胎儿畸形筛查就诊于当地医院怀疑胎儿椎管内占位,遂转诊至我院。产前超声检查:胎儿腰段及骶段椎管增宽,脊柱矢状切面发现腰骶部后方探及强回声团,后伴声影,凸入椎管且脊髓圆锥末端平第2骶椎水平,脊柱横断面似可见两束脊髓回声,胎儿小脑形态正常、后颅窝池及各脑室未见明显异常(图1)。超声提示:脊髓异常改变考虑脊髓纵裂合并脊髓栓系综合征。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#产前超声#
75
#纵裂畸形#
73
很少见
108
#畸形#
71
#产前#
93
#超声诊断#
79
#超声诊断#
55