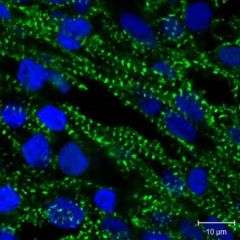
J Endod:三维球形培养使牙髓细胞具有独特的多能潜力
2017-06-18 lishiting MedSci原创
间充质干细胞(MSCs)是典型的利用传统组织培养方法进行单层融合式的培养。然而,此种技术在体内微环境中会使干细胞不完全生长,最终导致细胞的干性丧失。三维(3D)球形培养是最广泛应用于体内微环境的3D培养技术之一。然而,经过三维球形培养的牙髓干细胞(DPSCs)的细胞干性和多向分化能力还未完全清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#牙髓#
78
#牙髓细胞#
102
感谢分享一下,
1
#髓细胞#
91
感谢分享一下
113
三维培养应该是干细胞的活力会进一步增加这是必然的
98
好文章就值得拥有
96