J Clin Oncol:ESMO 氟维司群在晚期乳腺癌内分泌治疗中的新近进展
2017-09-24 佚名 肿瘤资讯
针对于激素受体阳性晚期乳腺癌患者,内分泌治疗一直是重要的治疗方法,相比化疗,内分泌治疗有着可靠的疗效及良好的生存质量。氟维司群是一种选择性雌激素受体下调剂,用于在抗雌激素辅助治疗后或治疗过程中复发的,或是在抗雌激素治疗中进展的绝经后(包括自然绝经和人工绝经)雌激素受体阳性的局部晚期或转移性乳腺癌。2017年FDA根据其FLACON研究的阳性结果,批准了氟维司群用在既往未接受内分泌治疗的,绝经后HR
在今年ESMO 关于晚期乳腺癌的报道中,有两项重要研究值得关注,分别是:BCRG-C06 Safari研究的亚组分析以及 monarch-2 的探索性分析。
JBCRG-C06 Safari研究的亚组分析是在JBCRG-C06 Safari研究的基础上,探索在亚组分析中影响氟维司群治疗晚期乳腺癌的TTF(肿瘤治疗失败时间)相关 因素。JBCRG-C06 Safari研究(UMIN000015168)显示氟维司群500mg在较早线使用的话,从诊断到疾病进展的时间较长。HR+的转移性/晚期乳腺癌患者中,没有接受过化疗的,其TTF有明显延长。本次亚组分析希望通过进一步数据分析,寻找两个亚组与延长的TTF相关的临床因素。两个亚组分别是HR+/HER2-和HR+/HER2+。选用的人群是氟维司群用于2线及2线以上内分泌治疗,研究因素包含年龄、治疗线数、氟维司群治疗时间、辅助化疗、组织学分级、内脏转移、ER表达、PR表达。采用Kaplan-Meier分析,使用单变量和多变量分析TTF。采用Cox风险比例模型评估每个临床因素和TTF之间的相关性。双侧检验,P ?0.05有统计意义。
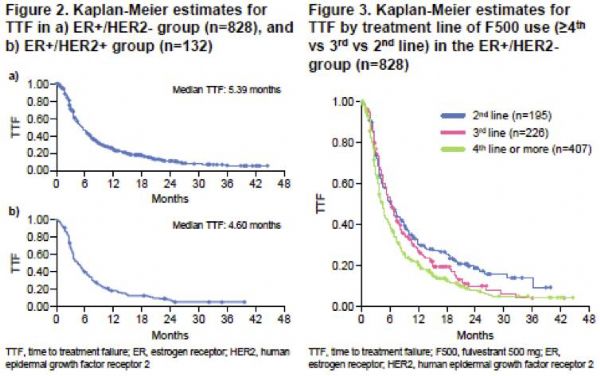
Safari研究从2011年11月至2014年12月在日本16个研究中心纳入了接受氟维司群500mg治疗的1072例患者。 其中828例ER + / HER2-和132例ER + / HER2 +患者符合纳入亚组分析。
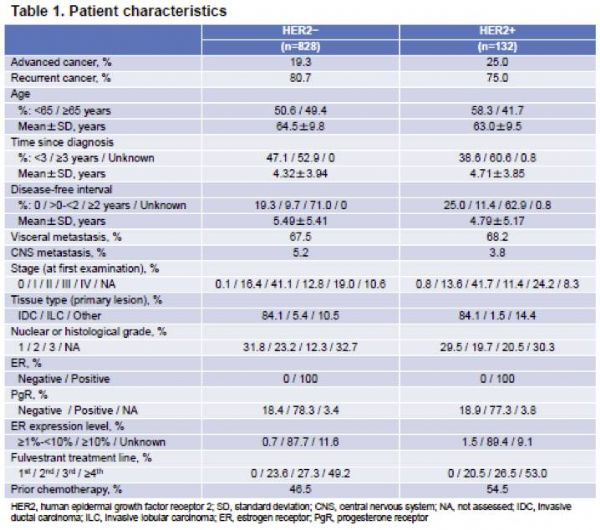
ER+/HER2?亚组的中位PFS为5.39个月,单变量分析显示,老龄、早线使用、无化疗和TTF延长有明显相关性。内脏转移和PgR表达对TTF无影响。多变量分析显示,老龄、从诊断到开始氟维司群治疗时间较长的、未接受化疗、氟维司群使用线数影响TTF。氟维司群500mg二线治疗TTF≥24个月的约18%,而≥3线治疗,TTF≥24个月的降低到10%以下。
ER + / HER2 +亚组的中位TTF为4.60个月。 单变量分析显示,治疗线数是与TTF延长的唯一相关因素。 在多变量分析中,各因素未显示与和TTF有相关性。
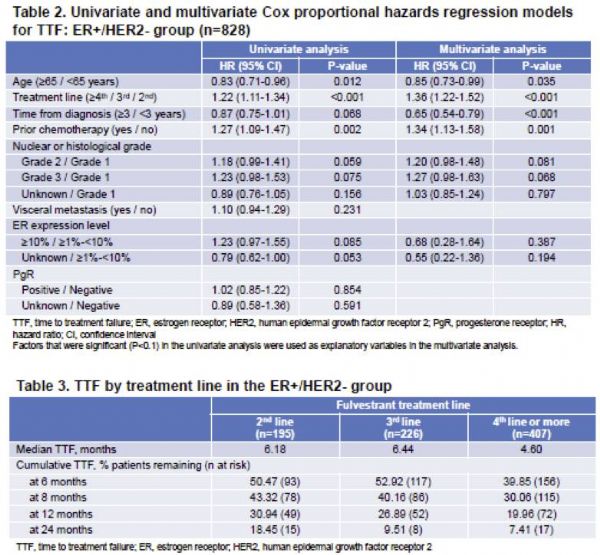
该亚组分析的一个重要目的是将Safari研究的数据与FALCON研究的数据进行比较,聚焦在是否存在内脏转移,PgR的表达,ER表达水平和针对晚期乳腺癌的化疗。本研究中的单变量分析显示,无论内脏转移或PgR状态如何,其TTF结果与FALCON亚组分析类似。本研究的亚组分析仅包括氟维司群用于二线及更晚线的治疗,而FALCON研究的入组患者是之前未接受内分泌治疗。
氟维司群的治疗线数与其TTF相关,这与其他研究结果一致,前线内分泌治疗影响其后线治疗的结果。本研究的结果可能有助于确定最有可能从氟维司群500mg治疗中获益的患者。
尽管该研究样本量较大,但因为是回顾性研究,患者在某些基线特征可能存在不平衡,在数据分析上有一定局限性,无法改变临床实践。但是,在本研究结果提示老龄、诊断为晚期或转移性乳腺癌至使用F500的时间间隔较长、未接受化疗、治疗线数较前,氟维司群500mg疗效更好。这些患者肿瘤进展缓慢,属于内分泌治疗的优势人群。
另一篇是氟维司群作为内分泌治疗基石类药物联合CDK4/6抑制剂Abemaciclib的研究,在未接受过内分泌治疗的HR+/HER2-晚期乳腺癌患者中,Abemaciclib联合氟维司群的MONARCH 2的探索性研究。
辅助内分泌治疗(ET)是ER/PgR阳性早期乳腺癌的标准治疗方式。然而,还是有大量患者复发或未接受辅助内分泌治疗。 此外,约5-10%的乳腺癌患者首诊就是晚期转移性疾病。(这些复发和首诊晚期的患者都属于内分泌耐药的转移性乳腺癌患者。)各种数据表明,之前的内分治疗方案等影响其晚期内分泌治疗的疗效。与阿那曲唑相比,氟维司群在局部晚期或转移性乳腺癌(MBC)具有优异的疗效。
雌激素激活细胞周期蛋白 D1,促进CDK4/6激活及细胞周期进展。CDK4/6短期抑制导致G1期停滞,使得细胞周期暂时停滞。Abemaciclib是一种持续口服的CDK4/6抑制剂。2017年ASCO报道了MONARCH 2研究,既往内分泌治疗后发生进展的HR+/HER2-晚期乳腺癌患者,Abemaciclib+氟维司群显着改善PFS(16.4 vs 9.3个月。基于MONARCH 1和MONARCH 2试验的优异结果,美国FDA已经接受新药abemaciclib的申请,并授予它优先审评资格。
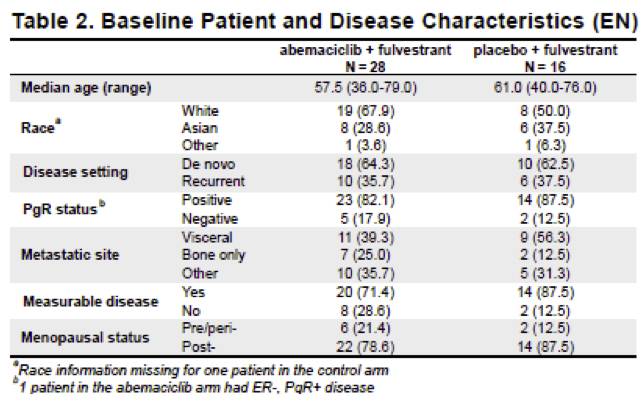
本试验是一项探索性研究,纳入了44例未经内分泌治疗的HR+/HER2-的晚期乳腺癌患者,MBC期间未接受化疗,从未接受过内分泌治疗,按2:1的比例分为Abemaciclib+氟维司群组和安慰剂+氟维司群组。
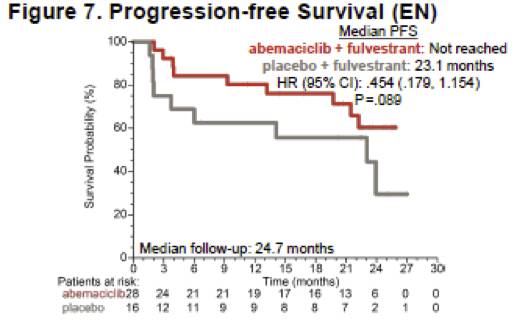
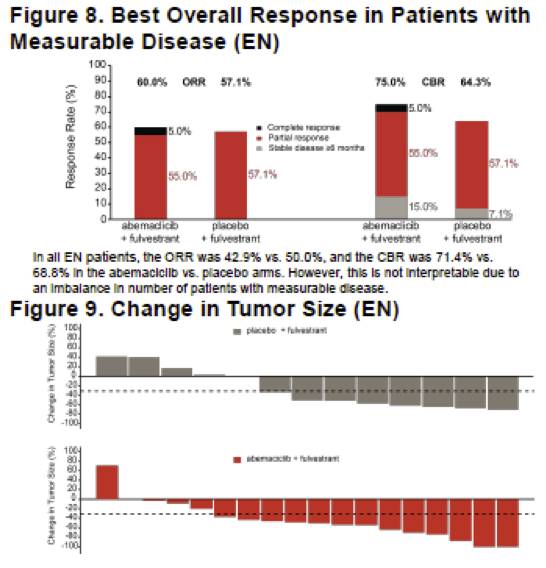

本研究获得了非常可喜的结果,但需要注意的是这是一个很小的样本量的探索性研究,还需要更大样本量的验证性试验结果。
MONARCH2研究和本次ESMO报道的相关探索性研究,结果显示在HR+/HER2-晚期乳腺癌患者,内分泌单药-氟维司群也取得了很好的疗效。MONARCH2纳入的是既往ET治疗时或完成后1年内发生进展,针对晚期未接受过化疗,允许有一线内分泌治疗的患者,氟维司群组的中位PFS是9.3个月,样本量223例。本次探索性研究纳入的是未经内分泌治疗的患者,针对晚期未接受过化疗,氟维司群组的中位PFS时23.1个月,样本量16例。在晚期内分泌治疗中,单用内分泌治疗取得的疗效令人振奋。内分泌治疗如果选对了合适的患者,不仅有良好的生活质量,也有更长的生存获益。激素受体阳性晚期乳腺癌治疗道路任重道远,内分泌治疗是主要治疗,对合适的患者进行适合的治疗,内分泌单药治疗及内分泌联系靶向治疗的获益人群特征,会让患者能有更多的受益,期待我们能拨开云雾观真颜。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#分泌#
68
#Oncol#
0
#SMO#
77
学习一下很不错
105
学习了.谢谢分享
85
#ESMO#
63