European Urology:冲击波碎石vs输尿管镜下取石,到底选哪个?
2021-06-24 MedSci原创 MedSci原创
尽管SWL是一种门诊无创治疗,对患者和减少住院医疗资源的使用都有潜在优势,但该试验显示,与SWL相比,URS在总体临床结果方面有好处,也反映在了当代临床中的实践。
肾结石发病率在全球范围内呈逐步上升趋势,这些病人通常是急诊科的常客,常常会被收入院治疗,最终可能需要积极的外科干预。在紧急情况下,肾结石可通过临时肾造口术或输尿管支架引流,而碎裂结石的最终手术治疗可采用冲击波碎石术(SWL)或输尿管镜激光碎石术(URS)。
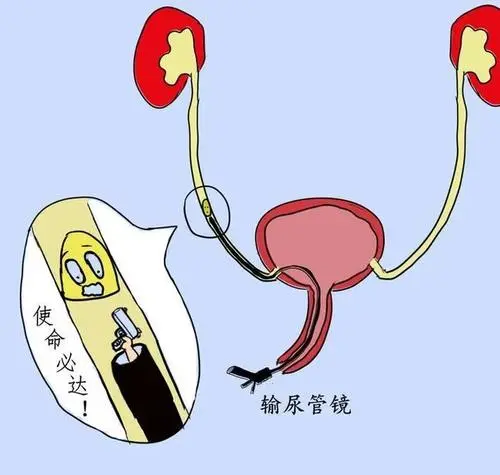
SWL可在门诊治疗(使用固定位或移动碎石机),而URS通常需要全麻并在手术室进行。尽管这两种治疗方式已经使用了20多年,但选择治疗方式通常是基于当地资源和专业知识、患者选择和可及性。
有研究者描述并报告了一项大型实用随机多中心研究的结果,该研究将SWL与URS(症状性输尿管结石治疗干预或TISU研究)进行了比较,以评估对患者具有重要意义的临床结果和次要转归指标,如生活质量,以便为患者、临床医生和卫生保健专员提供指导。这项研究分析近日发表在European Urology最新期刊上。
这项试验测试了两个疗程的SWL与URS作为输尿管结石初始治疗的非劣效性。主要结果是是否需要进一步干预以清除结石,次要结果包括生活质量评估、疼痛严重程度和严重并发症;这些研究是基于基线、8周和6个月时的问卷调查。研究者纳入了16年以上临床认为需要干预的单个输尿管结石患者。计划进行意向治疗分析和按方案分析。
该研究在2013年7月1日至2017年6月30日期间招募。从1291名符合条件的患者中招募了613名参与者,将306名参与者随机分为SWL组,307名参与者随机分为URS组。SWL组有67例(22.1%)需要进一步治疗,而URS组有31例(10.3%)。有利于URS的绝对风险差异为11.7%(95%可信区间5.6%,17.8%),在研究者为证明SWL非劣性设定的20%阈值内。
在试验中,研究者发现SWL组在6个月时的进一步干预率比URS组高11.7%(95%CI 5.6 17.8%),但这种差异并不差。也就是说,它在研究开始时设定的20%的限制范围内,以证明非劣效性。这将使患者和泌尿科医生能够接受它作为初始治疗途径。然而,通过对那些在治疗前没有清除或通过结石的患者进行的方案分析证明,URS可以更好地清除结石。
对患者和临床医生而言,在决定这些治疗途径时的一个关键因素是并发症。本研究中关注的是严重并发症,SWL(4%)和URS(3%)通路的并发症非常相似。
该RCT旨在检测SWL是否不逊于URS,并证实了这一点;尽管SWL是一种门诊无创治疗,对患者和减少住院医疗资源的使用都有潜在优势,但该试验显示,与SWL相比,URS在总体临床结果方面有好处,也反映在了当代临床中的实践。总之,本研究为输尿管结石(TISU)的治疗干预研究提供了新的证据,有助于指导这种常见健康状况的治疗方式的选择。
参考文献:Shockwave Lithotripsy Versus Ureteroscopic Treatment as Therapeutic Interventions for Stones of the Ureter (TISU): A Multicentre Randomised Controlled Non-inferiority Trial Ranan Dasgupta Sarah Cameron Lorna Aucott Sara J. MacLennan Kath Starr Sam McClinton Show all authors,DOI:https://doi.org/10.1016/j.eururo.2021.02.044
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#输尿管镜#
82
#PE#
75
#输尿管#
83
👍🏻
84