Molecular cell:高血压药物开发新契机 单基因调控血压
2015-05-12 佚名 生物谷
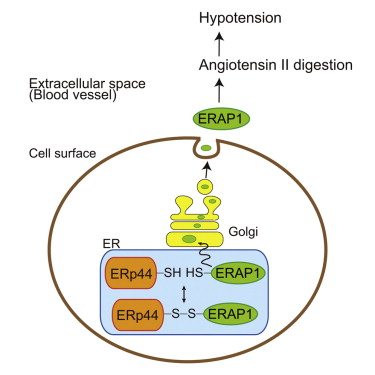
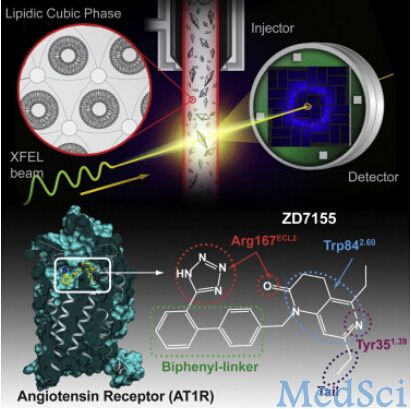
近日,来自日本理化研究所的研究人员在国际学术期刊molecular cell发表了一篇文章,对血压调控机制进行了深入探讨。高血压是导致中风,心脏病和糖尿病的重要风险因素,了解自然状态下身体如何调节血压对于开发治疗高血压的方法策略,将血压控制在正常水平具有重要意义。 在该项研究中,来自日本理化研究所的研究人员发现一个定位在内质网的多功能蛋白--ERp44缺失小鼠血压低于正常血压
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
62
#Cell#
65
#药物开发#
81
#基因调控#
119
看看
155