BMJ:韩国甲状腺癌的“流行”与其进行的甲状腺肿瘤筛查有关
2016-12-01 xing.T MedSci原创
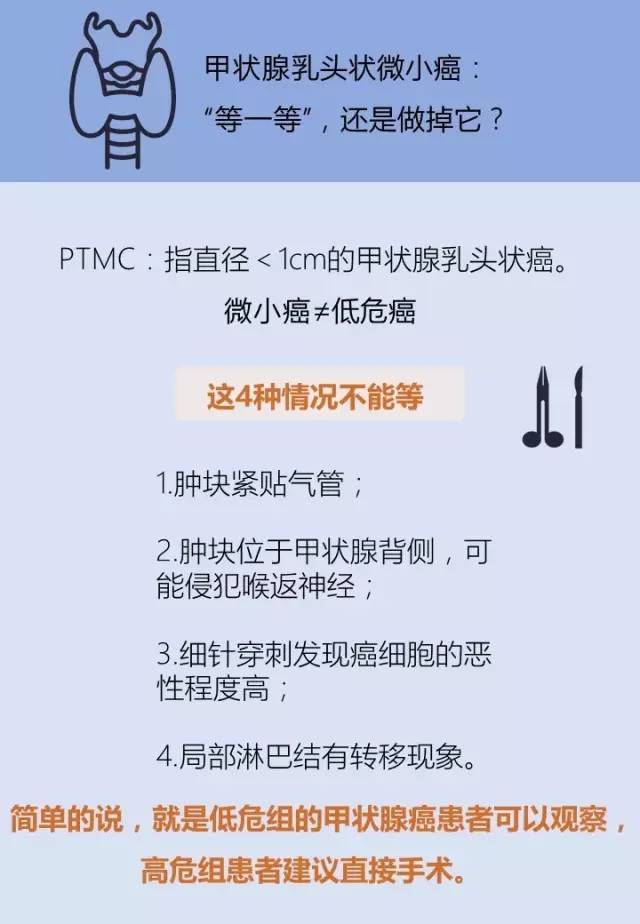
目前韩国“流行”的甲状腺癌是由于在对小肿瘤检测能力提高导致的,很有可能是过度检测的结果。在对无症状的一般人群减少不必要的甲状腺超声检查上,全国协调一致的努力是必要的。
最近,顶级医学杂志BMJ上发表了一篇来自韩国国立癌症中心国家癌症研究所的Sohee Park副教授及其研究团队的文章,旨在探讨韩国甲状腺癌的“流行”是否因韩国现在进行的甲状腺肿瘤筛查导致的。
在该研究中,研究人员通过审查具有全国代表性样本中分别在1999年、2005年和2008年被诊断为甲状腺癌患者的医疗记录。研究人员将人群按地区分层后采用系统抽样的方法从韩国全国癌症登记处随机抽取样本病例。
该项目的参与者包括5796例甲状腺癌患者(891例在1999年被诊断,2355例在2005年被诊断和2550例在2008年被诊断)。
主要结局指标为年龄标准化的甲状腺癌发病率和从1999年至2008年期间根据所用的甲状腺肿瘤检测方法(筛查与临床检测与非特异性检测)导致的发病率变化情况。
在1999年至2008年期间,甲状腺癌发病率增加了6.4倍(95%可信区间为4.9倍-8.4倍),从每100,000人6.4例(95%可信区间为6.2-6.6例)上升至每100,000人40.7例(40.2-41.2例)。在增加的肿瘤患者中,94.4%(每100,000人34.4例)患者肿瘤小于
由此可见,目前韩国“流行”的甲状腺癌是由于在对小肿瘤检测能力提高导致的,很有可能是过度检测的结果。在对无症状的一般人群减少不必要的甲状腺超声检查上,需要全国协调一致的努力。
原始出处:
Sohee Park,et
al. Association between screening and the thyroid cancer “epidemic” in
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#甲状腺肿瘤#
84
#BMJ#
84
#甲状腺肿#
85
继续学习
103
继续关注
103
继续学习
87
#韩国#
0
#肿瘤筛查#
98