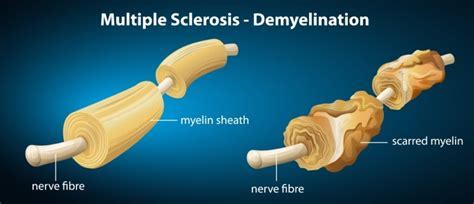
JAMA Neurol:继发性进行性多发性硬化症患者持续接受免疫治疗可降低残疾进展风险
2020-08-10 MedSci原创 MedSci原创
对于继发性进行性多发性硬化症患者积极接受疾病修饰治疗可改善残疾结局
近日研究人员就继发性进行性多发性硬化症(SPMS)接受疾病修饰疗法与残疾累积率之间的关系进行了考察。
本次研究为观察性队列研究,总计收集4997名SPMS患者数据,其中对1621例患者进行了充分随访并纳入数据分析,考察SPMS患者复发与残疾积累率的关系,并评估在第二进展期之前或期间的治疗是否能缓解残疾积累的进展。研究的主要终点以SPMS患者残疾积累为衡量指标,分析了两种结果:第二进展阶段的残疾累积率和轮椅依赖的风险。
1621患者中,1103例(68.0%)为女性,MS发病的平均年龄为33.9岁,共有661例患者(40.8%)在SPMS期间出现复发。对于复发缓解型多发性硬化患者,早期接受治疗不会增加复发或继发性进展期的残疾累积风险。在继发进行性疾病阶段,高复发率与轮椅依赖的风险增加相关(危险比[HR]:1.87)。在SPMS期间经历过叠加复发的患者中,积极接受疾病修饰治疗与降低残疾进展率和降低轮椅依赖风险显著相关。
研究发现,对于继发性进行性多发性硬化症患者积极接受疾病修饰治疗可改善残疾结局。
原始出处:
Nathaniel Lizak et al. Association of Sustained Immunotherapy With Disability Outcomes in Patients With Active Secondary Progressive Multiple Sclerosis.JAMA Neurol. July 27, 2020.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Neurol#
79
#多发性#
92
#进行性#
87
#继发#
100
#硬化症#
0
#残疾进展#
70
#继发性#
108
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
97