上皮性卵巢癌PARP抑制剂相关生物标志物有哪些?重点归纳!
2021-10-11 MedSci原创 MedSci原创
卵巢癌是女性生殖系统常见的恶性肿瘤,发病风险因素包括家族史、遗传因素、年龄、体质量、子宫 内膜异位症、未生育、激素替代治疗等。
卵巢癌是女性生殖系统常见的恶性肿瘤,发病风险因素包括家族史、遗传因素、年龄、体质量、子宫 内膜异位症、未生育、激素替代治疗等。由于缺乏有效的早期筛查手段,患者就诊时多为晚期,在中国卵巢癌患者的5年生存率约为40%。
近年来,随着聚腺苷二磷酸核糖聚合酶[poly(ADP-ribose)polymerase, PARP ] 抑制剂广泛应用于临床,有效地延长了晚期卵巢癌患者的无进展生存期。因此,对卵巢癌患者进行相关的生物标志物检测,有助于指导临床合理用药,改善卵巢癌患者的治疗结局。
PARP抑制剂相关的生物标志物
目前,与PARP抑制剂治疗相关的生物 标志物主要有BRCA1/2基因突变、HRR基因突变、 BRCA1/RAD51C启动子甲基化、HRD状态等。
1)BRCA1/2基因突变
BRCA1/2是重要的抑癌基因,对于维持细胞 正常的生长增殖至关重要,也是维持细胞HRR功 能最重要的基因。携带BRCA1/2突变的多种肿瘤 对PARP抑制剂敏感,在SOLO-1研究中,携带胚系或体细胞BRCA1/2突变的晚期上皮性卵巢癌患 者在初始治疗缓解后应用奥拉帕利维持治疗,相比安慰剂,患者复发或死亡风险下降70%,中位 PFS延长3年以上。
明确卵巢癌患者的BRCA1/2胚系突变状 态,有助于对患者及其家系进行遗传风险管理, 包括家系验证、制定筛查方案、化学预防、预防 性手术、生殖干预等。
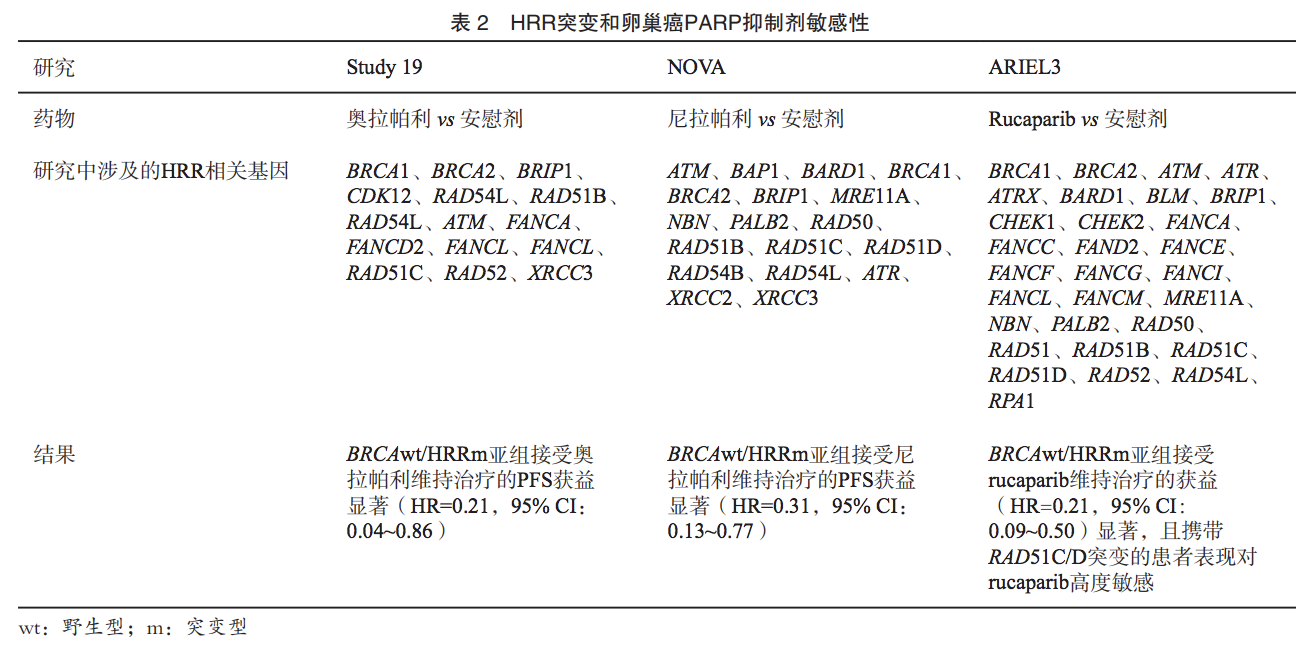
2)HRR基因突变
HRR是一个复杂的生物学过程,开始于细胞内 DNA损伤感应蛋白质对于DSB的识别,这个过程主 要依赖于MRN(MRE11、RAD50、NBS1)蛋白复 合物,随后在DNA酶的作用下由5’到3’对DNA进行 切割,ATM、RPA等蛋白结合于突出的单链DNA阻 止其进一步降解;以RAD51为核心的DNA重组酶 随后结合于单链DNA并在姐妹染色单体上寻找同源 序列以作为后续DNA修复的模板,在这个过程中, RAD51借由BRCA2募集到RPA结合的单链DNA上, 而BRCA2的募集则依赖于BRCA1和PALB2。
3)BRCA1/RAD51C启动子甲基化
基因的表观遗传学变化同样可能引起细胞发 生HRD,卵巢癌中较常见的是BRCA1和RAD51C 的启动子甲基化,BRCA1或RAD51C的甲基化将 导致对应的基因表达下调,并且通常与BRCA1/2 或其他HRR相关基因的变异互斥。
在患者来 源异种移植瘤(patient-derived xenograft,PDX) 小鼠模型、卵巢癌细胞系及PARP抑制剂的临床 研究中发现,BRCA1或RAD51C甲基化与rucaparib 的敏感性相关,纯合BRCA1甲基化对rucaparib 高度敏感,而杂合BRCA1甲基化对rucaparib表现出耐药。
4)HRD状态
在新诊断的卵巢癌中,BRCA1/2和HRD检测被推荐用于指导一线卵巢癌的治疗方案选择。除此之外,包括突变特征Signature 3、 HRDetect、功能性HRD检测(RAD51 Foci)等在 内的新兴生物标志物及检测方法对于PARP抑制剂敏感性的预测也在研究之中。
PARP抑制剂生物标志物检测建议
基于国内外指南及共识 的推荐、PARP抑制剂国内外药物适应证,以及 中国卵巢癌患者临床诊疗现状,经过专家组讨 论,对中国卵巢癌患者PARP抑制剂相关的生物标志物检测进行如下推荐:
1)推荐所有非黏液性卵巢癌患者在初次病理学检查确诊时,明确肿瘤BRCA1/2的突变 (包括胚系和体细胞突变)状态,对于Ⅰ期患者仅需明确胚系BRCA1/2突变状态(1类)。具体如下:
① 如果患者仅行肿瘤组织BRCA1/2检测,且突变 状态为阳性,建议进一步采用血液或唾液样本 进行BRCA1/2胚系检测,以明确该变异是否为 胚系变异(1类)。② 如果患者仅行肿瘤组织 BRCA1/2检测,且突变状态为阴性,建议进一 步对血液样本进行大片段重排(large genomic rearrangement,LGR)变异的检测以明确是否存 在BRCA1/2的胚系LGR变异(1类)。③ 如患者 仅行胚系BRCA1/2检测,且结果为阳性,则无需 再对肿瘤组织进行BRCA1/2检测(1类)。④ 如 患者仅行胚系BRCA1/2检测(包含针对LGR的 MLPA检测),且结果为阴性,则需要对肿瘤组 织进行BRCA1/2检测(1类)。⑤ 根据当地检测 策略并综合成本效益,可以同时进行BRCA1/2的 胚系及肿瘤突变检测,或胚系、肿瘤检测序贯进 行(2A类)。
2)对于新诊断的晚期卵巢癌患者(目前主要 证据在高级别浆液性卵巢癌和高级别子宫内膜样 癌),HRD状态(包括BRCA1/2和HRD score) 有助于医师选择不同维持治疗方案以期达到最佳治疗效果:
① 建议进行HRD检测(包括BRCA1/2和HRD score)(2A类);如患者存在抗血管生成抑制 剂治疗的禁忌证,或不考虑抗血管生成抑制剂 治疗时,HRD状态对于维持治疗的疗效预测及 预后判断仍有参考价值(2B类)。② 如既往接 受过肿瘤BRCA1/2检测,且结果为阳性,不需要 再补充进行HRD检测(1类)。③ 如既往接受过 肿瘤BRCA1/2检测,且结果为阴性,建议对肿瘤 样本进行HRD检测以明确是否为HRD阳性(2A 类)。④ 当HRD检测不可及时,可考虑对肿瘤 组织进行HRR基因检测(3类)。
3)对于铂敏感复发的卵巢癌患者,BRCA1/2 突变状态及HRD状态并不作为含铂类药物化疗后 PARP抑制剂维持治疗的选择标准,但对于患者 疗效预测及预后判断具有一定的参考价值:
① 既往已经接受过BRCA1/2或HRD的检测, 即便有更新的肿瘤样本可及时,也暂不推荐对 同一检测项目重复进行检测(2A类)。② 可考 虑进行HRD检测(包括BRCA1/2和HRD score) (2B类)。③ 如既往接受过肿瘤BRCA1/2检测, 且结果为阳性,不需要补充HRD检测(1类)。 ④ 如既往接受过肿瘤BRCA1/2检测,且结果为阴 性,可考虑进行HRD检测(2B类)。⑤ 当HRD 检测不可及时,可考虑进行肿瘤组织HRR基因检 测(3类)。
4)对于考虑使用PARP抑制剂作为单药挽救 性治疗的后线卵巢癌患者:
① 既往已经接受过BRCA1/2或HRD的检测, 即便有更新的肿瘤样本可及时,也暂不推荐对同 一检测项目重复进行检测(2B类)。② 铂敏感 复发的患者,推荐进行HRD检测(包括BRCA1/2 和HRD score)(2A类)。③ 铂耐药复发的患 者,仅需接受胚系和(或)肿瘤BRCA1/2检测 (2A类)。④ 当HRD检测不可及时,可考虑进 行肿瘤组织HRR基因检测(3类)。
参考来源:
中国抗癌协会妇科肿瘤专业委员会,中华医学会病理学分会.上皮性卵巢癌PARP抑制剂相关生物标志物 检测的中国专家共识.《中国癌症杂志》2020年第30卷第10期.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#皮性卵巢癌#
52
#上皮性卵巢癌#
60
#标志物#
42
#抑制剂#
50
学习了
73
#生物标志#
54
#生物标志#
41
#PARP#
53
学习了
71