Mol Pharmacol:研究人员发现双酚A对钙离子通道的不利影响
2013-05-06 Beyond 生物谷
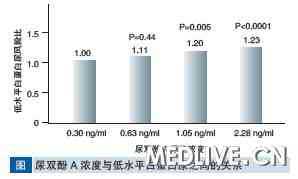
许多人工合成产品中发现的一种物质双酚A被认为是有害的,特别是对胎儿和婴儿。波恩大学研究人员在实验中已经表明这种环境化学物质能阻断人类和小鼠的组织细胞膜上的钙离子通道。研究结果发表在Molecular Pharmacology杂志上。 工业化学品双酚A(BPA)是全世界广泛用于制造聚碳酸酯树脂和合成树脂的材料。这种物质已被证明会影响内分泌系统,对酶和载体蛋白的功能可能产生负面影响。 BPA与心脏
许多人工合成产品中发现的一种物质双酚A被认为是有害的,特别是对胎儿和婴儿。波恩大学研究人员在实验中已经表明这种环境化学物质能阻断人类和小鼠的组织细胞膜上的钙离子通道。研究结果发表在Molecular Pharmacology杂志上。
工业化学品双酚A(BPA)是全世界广泛用于制造聚碳酸酯树脂和合成树脂的材料。这种物质已被证明会影响内分泌系统,对酶和载体蛋白的功能可能产生负面影响。
BPA与心脏病,糖尿病,肥胖,癌症和神经功能障碍相关。胎儿和新生儿对BPA特别敏感。由于其不可预测的影响,2011年欧盟委员会婴儿奶瓶禁止使用BPA。
研究人员现在报告说,双酚A阻断多个必需的钙离子通道,BPA能可逆性地阻断小鼠和人类细胞的钙通道。
钙离子流经这些孔状的蛋白通道进入活细胞,例如控制心脏肌肉细胞,酶的活性以及神经细胞的收缩。新研究表明,BPA的确可以对人体健康产生不利影响。由于双酚A是可逆的结合钙通道,研究人员相信该物质至少有从体内被清楚的可能性。

doi:10.1124/mol.112.081372
PMC:
PMID:
Bisphenol A Inhibits Voltage-activated Ca2+ channels In Vitro: Mechanisms and Structural Requirements
Andre Deutschmann1, Michael Hans1, et al.
Bisphenol A (BPA), a high volume production chemical compound attracts growing attention as health relevant xenobiotic in humans. It can directly bind to hormone receptors, enzymes and ion channels to become biologically active. In this study we show that BPA acts as a potent blocker of voltage-activated Ca2+channels. We determined the mechanisms of block and the structural elements of BPA essential for its action. Macroscopic Ba2+/ Ca2+currents through native L-, N-, P/Q-, T-type Ca2+channels in rat endocrine GH3 cells, mouse DRG neurons or cardiac myocytes and recombinant human R-type Ca2+channels expressed in HEK293 cells were rapidly and reversibly inhibited by BPA with similar potency (EC50 values: 26 to 35 μM). Pharmacological and biophysical analysis of R-type Ca2+ channels revealed that BPA interacts with the extracellular part of the channel protein. Its action does not require intracellular signaling pathways, is neither voltage- nor use-dependent and does not affect channel gating. This indicates that BPA interacts with the channel in its resting state by directly binding to an external site outside the pore forming region. Structure-effect analyses of various phenolic and bisphenolic compounds revealed that (i) a double-alkylated (R-C(CH3)2-R, R-C(CH3)(CH2CH3)-R), or double-trifluoromethylated sp3 hybridized carbon atom between the two aromatic rings and (ii) the two aromatic moieties in angulated orientation are optimal for BPA's effectiveness. Since BPA highly pollutes the environment and is incorporated into the human organism our data may provide a basis for future studies relevant for human health and development.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#pharma#
76
#MAC#
78
#Pharm#
75
#研究人员#
60
#钙离子#
76
#Pharmacol#
107
#双酚A#
82
#离子通道#
103