Cell Reports:科学家发现埃博拉病毒对免疫系统的早期影响
2017-01-22 佚名 生物谷
NIH的科学家使用一种新的早期埃博拉病毒(EBOV)感染的小鼠模型发现了免疫系统的早期免疫反应如何影响埃博拉病毒的发展。这个模型将有助于找到开发治疗EBOV感染药物的靶点。 来自美国NIH过敏和感染疾病研究所的科学家领导了这项研究,并与来自华盛顿大学和哥伦比亚大学的科学家一起合作完成。 科学家们分析了宿主细胞驱使免疫系统应对EBOV感染的信号通路及免疫系统由此产生的免疫反应。他们主

NIH的科学家使用一种新的早期埃博拉病毒(EBOV)感染的小鼠模型发现了免疫系统的早期免疫反应如何影响埃博拉病毒的发展。这个模型将有助于找到开发治疗EBOV感染药物的靶点。
来自美国NIH过敏和感染疾病研究所的科学家领导了这项研究,并与来自华盛顿大学和哥伦比亚大学的科学家一起合作完成。
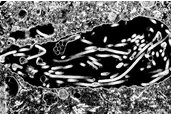
科学家们分析了宿主细胞驱使免疫系统应对EBOV感染的信号通路及免疫系统由此产生的免疫反应。他们主要关注了感染后数小时内发生的涉及细胞线粒体抗病毒信号蛋白(MAVS)的信号通路。
科学家们已经知道MAVS发挥着关键的抗EBOV效应,而这项研究是首次在动物模型中检测这个蛋白的作用。尽管许多细胞都可以产生MAVS,但是他们发现巨噬细胞产生的MAVS在控制EBOV感染及由此导致的器官和组织损伤中发挥重要作用。
在他们的实验中,巨噬细胞协调产生了最强烈的免疫反应,并且产生了1型干扰素,而1型干扰素是一种发挥抗病毒效应的重要蛋白。他们还发现EBOV可以抑制MAVS信号及干扰素的产生,从而引起感染小鼠患病。
为了能够最终开发出相关药物,科学家们将继续深入研究,以阐明MVOS控制的具体免疫反应及其机制,同时研究清除EBOV延缓免疫反应的机制。
原始出处
M Dutta et al.A systems approach reveals MAVS signaling in myeloid cells as critical for resistance to Ebola virus in murine models of infection.Cell Reports.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#埃博拉病#
94
#科学家发现#
60
#CEL#
92
#Cell#
89
#埃博拉病毒#
103