J INTERN MED:因怀疑急性心肌梗死入院但出院时为其它诊断的患者长期预后较差
2021-02-15 MedSci原创 MedSci原创
入院时怀疑心肌梗死(MI)但出院时未确诊心肌梗死的患者特征和预后尚未得到很好的归纳。近日,内科学领域权威杂志Journal of Internal Medicine上发表一篇研究文章,研究人员旨在比较
入院时怀疑心肌梗死(MI)但出院时未确诊心肌梗死的患者特征和预后尚未得到很好的归纳。近日,内科学领域权威杂志Journal of Internal Medicine上发表一篇研究文章,研究人员旨在比较出院时确诊或未确诊MI患者的基础特征和心血管结局。
吸氧在疑似急性MI中作用(DETO2X‐AMI)试验将6629名严重疑似AMI的患者随机分配接受吸氧或不吸氧,并进行比较。亚组分析的主要复合结局为2.1年随访期间的全因死亡、心肌梗死再住院、心衰(HF)或卒中的发生率(中位数,范围为1‐3.7年),不考虑随机治疗。
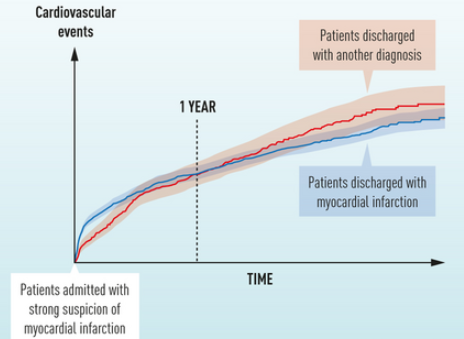
1619例(24%)患者出院时未被诊断为MI,5010例(76%)患者出院时被诊断为MI。两组患者在年龄上相似,但非MI患者多为女性,并有更多的合并症。第30天,复合结局在非MI患者中的发生率为2.8%(45/1619),而在所有单个终点发生率较低的MI患者中为5.0%(250/5010)。然而,在长期随访中,非MI患者的复合结局发生率增加到17.7%(1619例中有286例),而MI患者的复合结局发生率为16.0%(5010例中有804例),这主要是由更高的全因死亡、卒中和心衰发生率所致。
由此可见,因怀疑MI入院,但因另一种诊断出院的患者短期预后较好,但一年后,心血管结局和长期预后较差。
原始出处:
Bertil Lindahl.et al.Poor long‐term prognosis in patients admitted with strong suspicion of acute myocardial infarction but discharged with another diagnosis.J INTERN MED.2021.https://onlinelibrary.wiley.com/doi/10.1111/joim.13272
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#长期预后#
87
#Med#
141
好
120
学习了
160