Intensive Care Med:所有的危重病患者β-内酰胺类抗生素都应采用持续输注的方式给药吗?
2017-11-06 姚雯 重症医学
危重病患者中感染很常见,感染会导致ICU患者死亡率明显升高和患者医疗费用增加。严重感染的治疗手段之一是给予输注抗生素,然而,由于较迟识别特异的微生物以及越来越多的多重耐药病原体的播散,对临床医生来说,给予患者充分的抗生素治疗仍然是一个复杂的挑战。 国际指南中推荐对合并致命性感染的患者早期给予广谱抗生素治疗,特别是予以联合用药。 然而,优化危重病患者抗生素治疗时也要考虑药物的药代动力学特点(PK
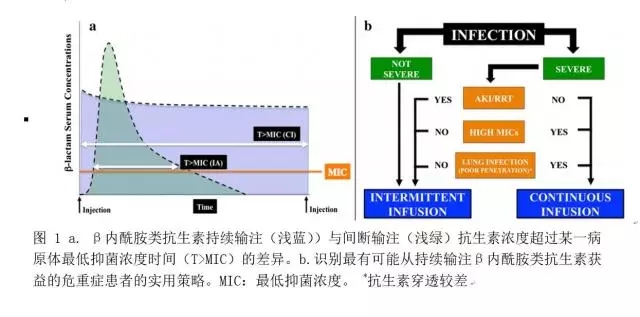
危重病患者中感染很常见,感染会导致ICU患者死亡率明显升高和患者医疗费用增加。严重感染的治疗手段之一是给予输注抗生素,然而,由于较迟识别特异的微生物以及越来越多的多重耐药病原体的播散,对临床医生来说,给予患者充分的抗生素治疗仍然是一个复杂的挑战。 国际指南中推荐对合并致命性感染的患者早期给予广谱抗生素治疗,特别是予以联合用药。 然而,优化危重病患者抗生素治疗时也要考虑药物的药代动力学特点(PKs),特别是与肾廓清增加及廓清减少有关的药物表观分布容积增加,而药物表观分布容积的变化与循环中抗生素水平的改变有关,循环中抗生素浓度不足可能会导致治疗失败。β-内酰胺类抗生素是重症感染的一线治疗药物,当其血药浓度超过病原体最低抑菌浓度的时间大于给药间隔时间时,药物治疗效果最佳。当按标准给药间隔给予危重病患者治疗时,药物的药代动力学特征会发生显著和无法预测的变化,而持续输注β-内酰胺类抗生素能使得几乎所有患者快速实现体内血药浓度超过病原体最低抑菌浓度的时间大于给药间隔,甚至一些对抗生素治疗不是那么敏感的病原体,比如铜绿假单胞菌和鲍曼不动杆菌,也能达到上述目标,因此,我们应该对危重症患者的每日用药方案进行优化(图1a)。但是,支持持续输注抗生素与标准治疗组相比也可改善预后的证据仍十分有限。
正因为如此,Abdul-Haziz等人进行了一项研究,研究结果最近发表在了重症监护医学杂志上, 他们对不需要肾脏替代治疗(RRT)的患者持续输注β-内酰胺类抗生素与标准的间断给予抗生素的治疗效果进行了评价,比较了两组患者中断抗生素治疗14天后的临床治愈率。该研究总共招募了140名患者,与标准的抗生素间断给药组相比,抗生素持续输注组患者的临床治愈率更高(56% vs 34%,p=0.01),无机械通气时间更长。 并且在治疗的第1天和第3天,与间断给药组相比,抗生素持续输注组中有更多患者达到合理用药的目标(例如:两次给药间隔之间的血药浓度均超过病原体最低抑菌浓度)(97% VS 70%, P<0.001)。 两组间14天和30天的死亡率未见差异。
那么我们应当对所有的危重感染患者均采用持续输注β-内酰胺类抗生素吗?也许并不是!之前的研究中出现了充满争议的结果,尽管在某些亚组患者中,持续输注β-内酰胺类抗生素可能对患者有益。 在DALI研究数据库中有一项研究纳入了182名患者,该研究发现与间断输注抗生素组相比,持续输注哌拉西林他唑巴坦或者美罗培南组患者30天存活率显著升高,但这一差异仅在呼吸系统感染的患者亚组中有统计学意义(86% vs 57%, P=0.01)。 实际上,尽管β-内酰胺类抗生素对肺组织的穿透相对有限,对于呼吸机相关肺炎患者而言,头孢他啶持续输注与抗生素间隔给药组相比,可在更短的时间内在肺内达到有效浓度,并且更易于对其药代动力学特点进行预测。 而该研究同样也表明与间断给药组相比,持续输注β-内酰胺类抗生素在重症患者中治疗效果更好(73% VS 35%, p=0.003)。 而在另一项针对由铜绿假单胞菌所致院内获得性肺炎的研究中,持续输注哌拉西林他唑巴坦仅在急性生理和慢性健康评估(APACHE)II评分大于17分的患者中显示出较间断给药组更低的14天死亡率。 另一个影响危重病患者抗生素持续输注治疗效果的重要混杂因素是病原体的特征。 用标准间断给予抗生素的方法足以消灭易感细菌,而且仅在那些对抗生素不敏感的菌株中存在β-内酰胺类抗生素浓度不足风险较高,比如说,那些MIC值较高的病原体,但其MIC值仍然在国际指南推荐意见认为对抗生素治疗有应答的范围内。Lorente等人所开展的一项回顾性研究的结果表明对于未合并肾衰竭的呼吸机相关肺炎患者的治疗而言,与间断给药组相比,持续输注哌拉西林他唑巴坦临床治愈率更显更高,但该治愈率的差异仅出现在分离得到的病原体MIC≥8mg/L时( 15/17 vs 7/21, P=0.002)。 最后需要关注的是药物蓄积,在一个大型感染患者的队列研究中,研究者给予患者持续或者间断输注β-内酰胺类抗生素,研究未发现两组患者90天死亡率(74% vs 73%,P=0.61)或者临床治愈率(52% VS 49%, P=0.56)有差异。然而,该研究并未测定患者体内的药物浓度,并且纳入了肾衰竭或者需要肾脏替代治疗的患者,而上述因素与药物蓄积相关,即使给予间断给药,这些患者体内抗生素浓度不足的风险还是较低的,这是该研究的一个重大偏倚。 另外,极高浓度的β-内酰胺类抗生素对危重病患者也是有害的,其潜在神经系统并发症的风险可能会超过控制感染所带来的获益。
重要的是,尽管Abdul-Haizz的研究报道了持续输注β-内酰胺类抗生素在严重脓毒症治疗中可带来巨大获益,我们仍然需要对该研究的一些重要的局限予以阐明。 首先,这是一个开放标签的临床试验。知晓治疗分配情况可能导致医生对患者采用不同的治疗方法,但更重要的是这可能会影响患者预后的评估。如果该研究能通过对分配方案不知情的裁决委员会对最后的结果进行评价,那么其研究质量则可显著提升。其次,该研究的作者并未对其分离得到病原体的真实MIC值进行报道,而仅仅借鉴已经发表的指南中病原体易感性的预测数据。而全世界不同地方同一病原体MIC值有很大差异,并且即使在同一地区的不同医院或者同一医院的不同时期该值均可有较大差异,这一事实对在临床中实施该治疗方法引发了一些严重的问题。此外,超过三分之一临床治愈的患者并未检出病原体,这就限制了医生对改善药物疗效所需血药浓度的计算。再次,该研究的作者发现了很大一部分难以治疗的病原体,而这不一定能反映易感模式不同的其他国家的病原体分布。 第四,该研究仅对血浆中的药物浓度进行了测定,这种持续输入的方法在处理如脑、腹腔或骨等药物穿透性差的部位的感染时可能会受到限制。 另外,该研究中绝大部分为呼吸道感染,无法据此得出持续静脉输注对其他类型的感染也可得到潜在获益的结论。第五,对治疗有应答者及治疗失败者中患者血药浓度大于MIC值的时间超过100%给药间隔时间的患者人数百分比是近似的。正因为如此,尽管抗生素持续输注也许能带来一些临床获益,但这些获益似乎与更长的抗生素暴露时间和更高的药物浓度无关。与治疗失败组相比,临床治愈患者的APACHE II的评分更低而且他们中更多的人接受了美罗培南治疗。因此,疾病严重程度不同以及抗生素的抗菌谱和杀菌活性的不同也对不同治疗组患者预后的差异产生影响。最后,没有研究提供新出现的耐药菌株和/或超级感染病原体相关的数据,尽管在临床实践中这一问题极难解决,而治疗这两种并发症可能也需要达到足够的血药浓度。
总之,大家仍然对危重病患者通过持续输注β-内酰胺类抗生素以优化其体内β-内酰胺类抗生素的浓度这一概念非常感兴趣,但是其目前尚未被有信服力的证据所证实。目前的证据表明最好对严重感染、肾功能正常和肺部感染患者采取这种治疗策略,并且分离到或者怀疑的病原体对抗生素不敏感(图1b)。未来需要针对持续输注β-内酰胺类抗生素对患者预后的影响进行进一步深入的研究,尤其是一些特殊情形,如患者接受肾脏替代治疗或者肾衰竭等额外的混杂因素可能会进一步改变机体内的药物浓度。
原始出处;
Taccone FS1, Laupland KB2, Montravers P3.Continuous infusion of β-lactam antibiotics for all critically ill patients?Intensive Care Med. 2016 Oct;42(10):1604-6. doi: 10.1007/s00134-016-4241-7. Epub 2016 Jan 29.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#危重病#
41
#TENS#
36
#β-内酰胺类#
49
#Med#
31
学习了谢谢分享!!
57
学习了.涨知识
46
学习了新知识
56
谢谢分享.学习了
57
好好好好好好好好
0