Heart:经导管二尖瓣修复的左心房压力正常患者特征和预后
2020-03-28 xiangting MedSci原创
TMVR时LAP正常与CLD发病率升高相关,而CLD可独立预测1年死亡率升高。
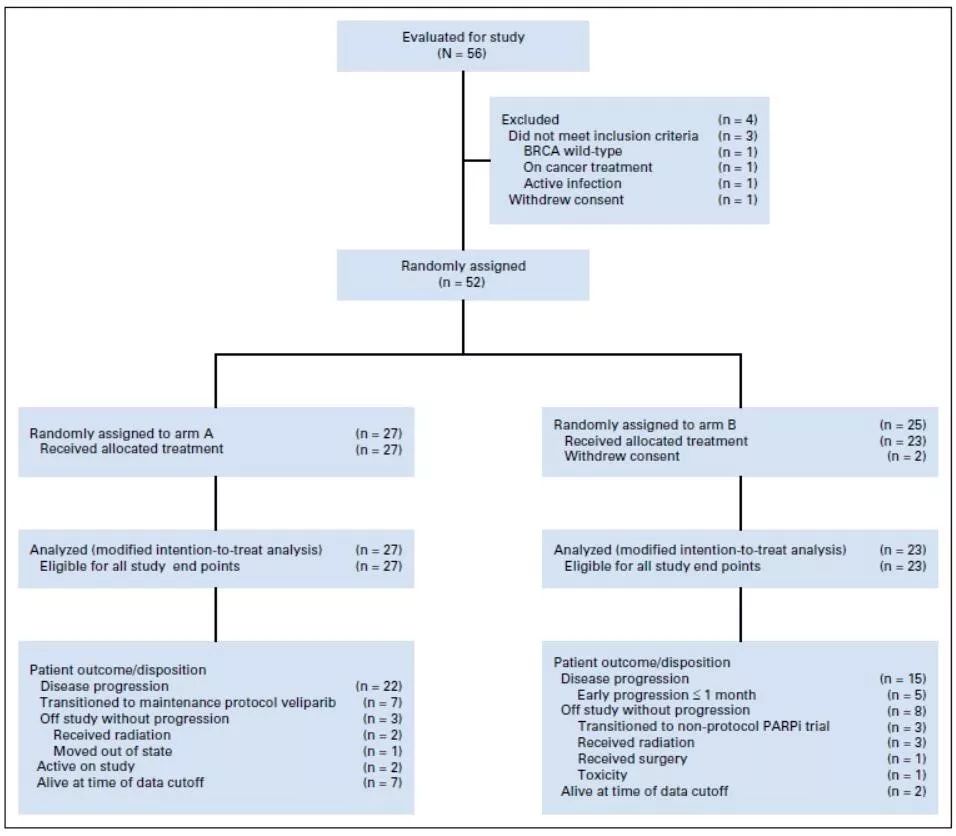
尽管有严重的二尖瓣返流(MR),部分患者在经导管二尖瓣修复(TMVR)时左心房压力(LAP)仍正常(<13mmHg)。这项研究目的是确定接受TMVR的LAP正常患者的临床特征和结局。
分析了一个于2014年5月1日至2018年5月1日接受经导管缘对缘二尖瓣夹和连续LAP监测的单中心回顾性连续患者队列。通过Kaplan-Meier生存曲线比较了1年死亡率。进行多因素分析以确定正常LAP和1年死亡率的预测因子。
204例接受TMVR的患者中,男性占65%,平均年龄为81岁。其中31例患者(15%)LAP正常(平均LAP为10.5mmHg,平均V波为16.5mmHg),而173例LAP升高(平均LAP为19mmHg,平均V波为32.5 mmHg)。尽管正常LAP组的有效返流孔面积和返流量明显较低,但两组间的严重MR患病率没有差异。组间的其他重要基线特征包括既往心脏手术、房颤、高血压、糖尿病、充血性心力衰竭、体重指数、MR机制和射血分数均相似。但是,正常LAP组的慢性肺病(CLD)患病率升高(45.2%vs 17.3%,p<0.001)。在多因素分析中,正常LAP的唯一重要预测指标是存在CLD(OR 4.79(1.83-12.36),p=0.001),正常LAP组的1年死亡率明显更高(32.3%vs 12.7%,p=0.006)。调整合并症后,正常LAP不再是1年死亡率的预测指标(RR 1.62(0.64-4.06),p=0.32);然而,CLD仍然是统计学显著的预测指标(RR 3.44(1.37-8.67),p=0.01)。
TMVR时LAP正常与CLD发病率升高相关,而CLD可独立预测1年死亡率升高。在CLD和严重MR患者中,测量LAP有助于确定那些从TMVR中获益可能性小的患者。
原始出处:
Jason R Sims. Characteristics and outcomes of patients with normal left atrial pressure undergoing transcatheter mitral valve repair. Heart. 22 March 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#二尖瓣修复#
47
#左心房#
61
#ART#
46
#二尖瓣#
58
#经导管#
51
#HEART#
42
#患者特征#
48
#心房#
46