18F-NaF PET/CT用于监测前列腺癌病情的展望
2015-03-03 cmt 中国医学论坛报
前列腺癌容易出现成骨性转移,但目前主要依靠监测PSA、99mTc-MDP骨扫描、CT,但诊断方法对多发骨转移非常有效,但是在肿瘤进展初期作用有限,而此时治疗有可能达到最佳的效果,因此有必要寻找能早期发现前列腺癌骨转移的手段。 18F-NaF PET/CT是一项针对前列腺癌骨转移比较敏感的检查。其原理是成骨性转移灶能摄取氟化钠18F-NaF,故能鉴别典型良性与恶性病变。与99mTc-MDP
前列腺癌容易出现成骨性转移,但目前主要依靠监测PSA、99mTc-MDP骨扫描、CT,但诊断方法对多发骨转移非常有效,但是在肿瘤进展初期作用有限,而此时治疗有可能达到最佳的效果,因此有必要寻找能早期发现前列腺癌骨转移的手段。
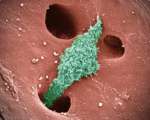
18F-NaF PET/CT是一项针对前列腺癌骨转移比较敏感的检查。其原理是成骨性转移灶能摄取氟化钠18F-NaF,故能鉴别典型良性与恶性病变。与99mTc-MDP进行骨扫描检查比较,18F-NaF PET/CT扫描有着较之高10倍的灵敏性,更高的空间分辨率,并能进行CT解剖定位及三维成像。因此,18F-NaF PET/CT成为早期发现前列腺癌骨转移的有效影像检查手段。目前,18F-NaF PET/CT检查的临床研究大都在进展期骨转移病人中进行。
研究发现,18F-NaF PET/CT检查虽能发现更多转移灶,但并不能改变临床治疗方案。同时发现,某些前列腺癌患者存在18F-NaF阳性灶,但CT扫描上未见骨质密度异常,能否将患者定义为转移,尚需结合其他临床特征判断(如肿瘤级别及大小、PSA水平等)。当氟化钠PET/CT阳性发现越多时,转移性疾病的可信度越高。部分研究者认为,18F-NaF PET/CT可替代99mTc-MDP骨扫描检测前列腺癌骨转移。
然而,现今国内外治疗指南尚将99mTc-MDP骨扫描作为标准的检查技术。由于18F-NaF PET/CT发现疾病进展而改变治疗方案的临床价值尚不明确,因此开展了一些研究以明确18F-NaF PET/CT的价值。如,18F-NaF PET/CT与全身MRI检测前列腺癌复发的Ⅱ期临床试验;18F-NaF PET/CT与传统骨扫描在肺癌、乳腺癌、前列腺癌中早期骨转移诊断中应用;前列腺癌、乳腺癌中18F-NaF PET/CT与SPECT骨扫描的作用;18F-NaF PET/CT在去势抵抗性转移性前列腺癌中重复性及治疗中评效价值(化疗或抗雄激素受体治疗);前列腺癌不同治疗疗效中的18F-NaF变化等。
总之,在转移性前列腺癌治疗快速发展的当下,18F-NaF PET/CT展示出了其临床可行性,尤其是早期转移灶诊断更具临床价值。我们尚需要从18F-NaF PET/CT相应的临床研究及其临床实践中总结出更多的经验,来检测18F-NaF PET/CT能否作为前列腺癌病情监测的有效手段。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#病情#
82
#PE#
82
很不错学习了
158
#PET/CT#
94
#PET#
77