JAMA Cardiol:科学家发现肺动脉高压致病新基因
2020-04-20 李羽壮 中国科学报
日前,北京协和医院心内科教授荆志成团队发现罕见病特发性肺动脉高压(IPAH)的全新疾病基因前列腺素合成酶(PTGIS),该基因的罕见变异可解释 6.1% 的 IPAH 患者病因。
日前,北京协和医院心内科教授荆志成团队发现罕见病特发性肺动脉高压(IPAH)的全新疾病基因前列腺素合成酶(PTGIS),该基因的罕见变异可解释 6.1% 的 IPAH 患者病因。研究同时发现,携带 PTGIS 罕见变异的患者对前列环素类药物治疗更为敏感,或可为临床精准用药提供指导。相关研究成果在线发表于《美国医学会杂志 · 心脏病学》。
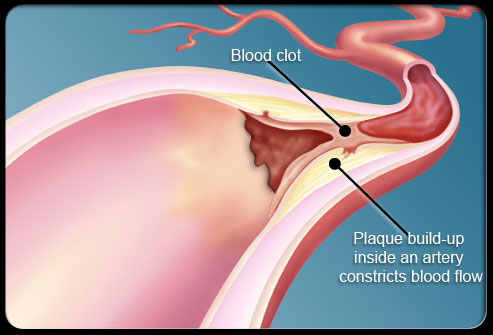
IPAH 是一种罕见恶性心血管疾病,病理机制不清,患者预后极差。BMPR2 是已知最主要的 IPAH 致病基因,但仅能解释 14.5% 的中国 IPAH 患者遗传病因,还有大量疾病相关基因未被揭示。
基于此,荆志成带领团队开展临床和基础研究。去年,该团队完成首次中国人大样本 IPAH 临床队列全基因组遗传研究,发现全新 IPAH 致病基因 BMP9,引起国际学术界高度关注。
《欧洲心脏杂志》曾此进行了长篇报道,介绍了该团队在心血管疾病的遗传学、队列研究以及新药研发方面取得的成就。
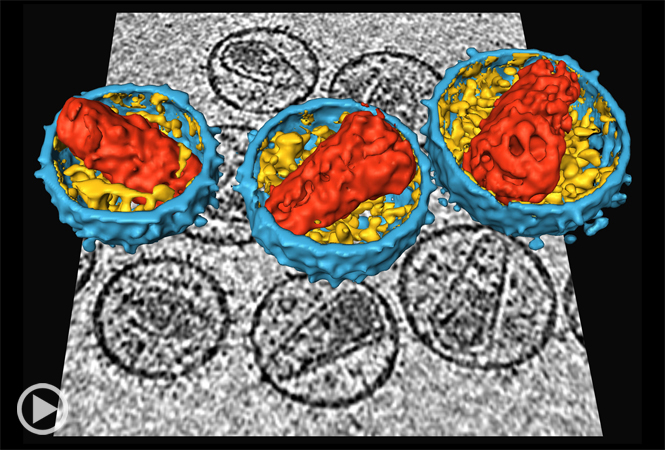
研究团队首先对 42 个不携带 BMPR2 突变的 IPAH 患者进行全基因组测序,发现 PTGIS 基因罕见变异在 IPAH 患者中显着聚集。随后,扩大样本的验证表明,PTGIS 基因罕见变异在 IPAH 患者中发生频率为 6.1%,显着高于健康对照人群 0.8% 的发生频率,使 IPAH 发病风险上升 7.8 倍。
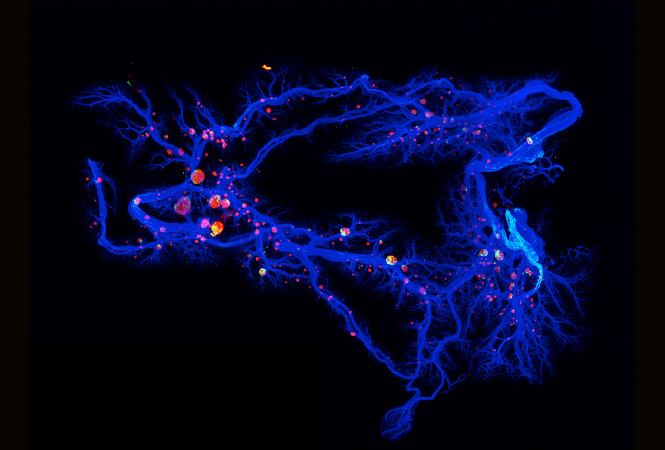
IPAH 患者中共发现 3 种 PTGIS 基因罕见变异:一个剪接位点变异(c.521+1G>A)和两个错义变异(p.R252Q 和 p.A447T)。功能研究表明这 3 种变异均导致 PTGIS 蛋白功能缺失:剪接位点变异导致错误 mRNA 剪接;两个错义变异均显着降低 PTGIS 蛋白合成前列腺素(PGI2)能力,也降低了 PTGIS 蛋白保护血管内皮细胞的功能,使血管内皮细胞更易凋亡和受损。
更让人兴奋的发现是,PTGIS 罕见变异与 IPAH 患者肺血管反应性具有很强相关性。线性回归模型研究表明,与不携带 PTGIS 罕见变异患者相比,携带罕见变异患者在吸入伊洛前列素后肺血管阻力下降更明显,心功能指数升高更明显。这意味着携带 PTGIS 罕见变异的患者对前列环素类药物的肺血管反应更敏感,很可能更适合进行前列环素类药物治疗,说明 PTGIS 罕见变异具有重要的指导临床治疗价值。
荆志成表示,PTGIS 基因罕见变异的发现是一个重大突破,不仅解释了额外 6.1%IPAH 患者的病因,亦可为临床精准用药提供指导。
原始出处:
Xiao-Jian Wang, et al. Association of Rare PTGIS Variants With Susceptibility and Pulmonary Vascular Response in Patients With Idiopathic Pulmonary Arterial Hypertension. JAMA Cardiol. Published online April 1, 2020. doi:10.1001/jamacardio.2020.0479.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cardiol#
77
#科学家发现#
75
#动脉高压#
64
#新基因#
93
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
87
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
81