NATURE:糖皮质激素促进乳腺癌转移
2019-03-16 海北 MedSci原创
转录组学,蛋白质组学和磷酸化蛋白质组学研究表明,糖皮质激素受体激活转移中的多个过程和激酶ROR1的表达增加,这两者都与存活率降低相关。
在疾病进展期间发展,肿瘤和转移瘤之间的多样性(称为患者内肿瘤异质性)是治疗的严重障碍。转移是癌症的致命标志,并且至今为止,转移级联中最复杂的步骤的定植机制仍然定义不明确。
更清楚地了解作为患者内肿瘤异质性和转移的基础的细胞和分子过程对于个性化癌症治疗的成功至关重要。
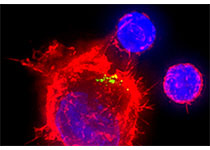
最近,使用小鼠中患者衍生的异种移植模型中的肿瘤和匹配的转移瘤的转录分析,研究人员发现,癌症位点特异性表型和远处转移中的糖皮质激素受体活性增加。
糖皮质激素受体介导应激激素和这些激素的合成衍生物的作用,这些激素在临床上广泛用作抗炎和免疫抑制剂。
研究人员表明,乳腺癌进展过程中应激激素的增加导致远处转移部位糖皮质激素受体的激活,定植增加和存活率降低。
转录组学,蛋白质组学和磷酸化蛋白质组学研究表明,糖皮质激素受体激活转移中的多个过程和激酶ROR1的表达增加,这两者都与存活率降低相关。
在临床前模型中,ROR1的消融减少了转移性生长,并延长了存活期。
该研究结果表明,糖皮质激素受体的激活增加了异质性和转移,这表明,当使用糖皮质激素治疗患有癌症相关并发症的乳腺癌患者时需要谨慎。
原始出处:
Obradović MMS et al. Glucocorticoids promote breast cancer metastasis. NATURE, 2019; doi: 10.1038/s41586-019-1019-4.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
58
#糖皮质#
63
嗯 不错 去找原文看啦
110
#癌转移#
58
#皮质激素#
86
不错
112