ATVB:细胞因子介导的转录因子 ERG 降解影响肺血管对全身炎症反应的反应
2023-06-18 刘少飞 MedSci原创 发表于上海
肺血管对细胞因子诱导的破坏敏感性是否是由影响内皮ERG保护肺ECs免受炎症损伤的组织学机制引起的。
研究背景
在感染性疾病中,促炎细胞因子会暂时破坏血管内皮细胞(ECs)之间的相互作用,以促进免疫分子和细胞进入组织。然而,在肺部,这种血管高通透性可能导致器官功能障碍。以前的研究发现转录因子ERG(红细胞前体转录因子相关基因)是内皮细胞稳态的主要调节因子。在这里,我们调查肺血管对细胞因子诱导的破坏敏感性是否是由影响内皮ERG保护肺ECs免受炎症损伤的组织学机制引起的。
研究方法
在培养的人脐静脉内皮细胞中分析细胞因子依赖的ERG泛素化和蛋白酶体降解。通过系统给予TNFα(肿瘤坏死因子α)或细菌细胞壁成分脂多糖,在小鼠中引起广泛的炎症挑战;通过免疫沉淀、免疫印迹和免疫荧光来评估ERG蛋白水平。通过遗传学方法在小鼠ECs(Ergfl/fl;Cdh5[PAC]-CreERT2)中诱导Erg的缺失,并通过组织学、免疫染色和电子显微镜分析多个器官。
研究结果
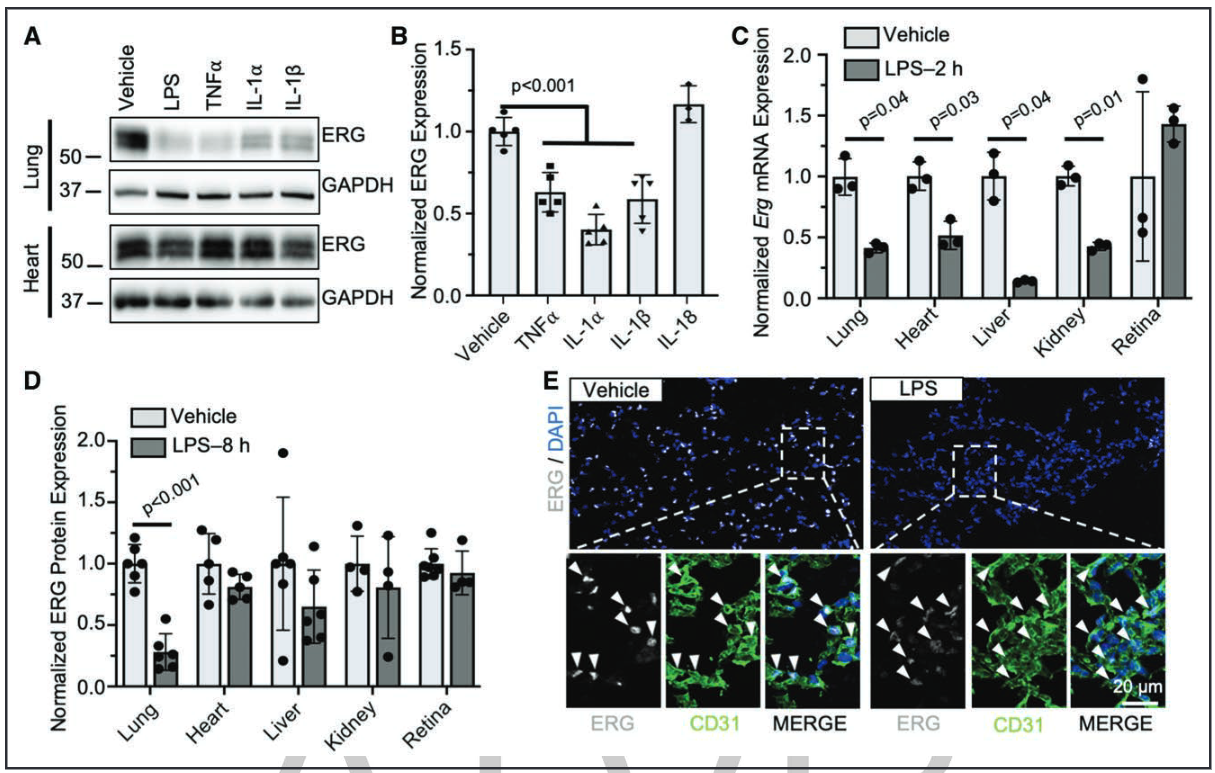
体外实验发现,TNFα促进了培养的人脐静脉内皮细胞中ERG的泛素化和降解,而蛋白酶体抑制剂MG132可以阻断这一过程。体内实验中,系统给予TNFα或脂多糖导致肺部内皮细胞内ERG的迅速而显著降解,但视网膜、心脏、肝脏或肾脏的内皮细胞没有受到影响。在小鼠流感感染模型中,肺部ERG的表达也下调。Ergfl/fl;Cdh5(PAC)-CreERT2小鼠自发地再现了炎症挑战的某些特征,包括以肺部为主的血管高通透性增加、免疫细胞的招募和纤维化。这些表型与肺部特异性下调的Tek表达有关,Tek是ERG的基因靶点,先前已与在炎症期间维持肺血管稳定性有关。
研究结论
总体而言,我们的数据突显了ERG在肺血管功能中的独特作用。我们认为,细胞因子诱导的ERG降解和随后在肺内皮细胞中的转录变化,在感染性疾病期间的肺血管不稳定中起着关键作用。
参考文献:
Schafer CM, Martin-Almedina S, Kurylowicz K, Dufton N, Osuna-Almagro L, Wu ML, Johnson CF, Shah AV, Haskard DO, Buxton A, Willis E, Wheeler K, Turner S, Chlebicz M, Scott RP, Kovats S, Cleuren A, Birdsey GM, Randi AM, Griffin CT. Cytokine-Mediated Degradation of the Transcription Factor ERG Impacts the Pulmonary Vascular Response to Systemic Inflammatory Challenge. l. 2023 Jun 15. doi: 10.1161/ATVBAHA.123.318926. Epub ahead of print. PMID: 37317853.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好文章,谢谢分享。
42
学习了,谢谢分享
48
pdkaocd
34
,促炎细胞因子会暂时破坏血管内皮细胞(ECs)之间的相互作用
47
不错 学习了
47