Liver Cancer:Atezolizumab (ATEZO) + bevacizumab (BEVA)一线治疗晚期HCC进展后,二线治疗选择对比
2021-11-28 yd2015 MedSci原创
肝细胞癌(HCC)是全球第四大癌症死亡原因。一半以上的HCC病例在诊断时处于晚期。自2008年以来,口服酪氨酸激酶抑制剂(TKI)索拉非尼(Sorafenib, SORA)已被推荐为BCLC C期(晚
肝细胞癌(HCC)是全球第四大癌症死亡原因。一半以上的HCC病例在诊断时处于晚期。自2008年以来,口服酪氨酸激酶抑制剂(TKI)索拉非尼(Sorafenib, SORA)已被推荐为BCLC C期(晚期)HCC患者和BCLC B期(中期)HCC患者的标准一线全身治疗。近期,研究表明atezolizumab (ATEZO) + bevacizumab (BEVA)方案较索拉非尼改善患者的OS和PFS,目前是一线治疗晚期肝细胞癌(HCC)的新标准。然而,在以免疫治疗为基础的一线治疗失败后,二线TKI治疗较安慰剂改善患者预后,但是二线治疗的最佳选择仍然不确定。因此,国外研究者开展了相关研究,基于现有的III期随机临床试验(RCT),以确定最佳的风险/受益顺序策略。相关研究结果发表在Liver Cancer杂志上。
研究构建了一个Markov模型来评估连续一线和二线系统治疗的总生存期(OS)。从一线ATEZO加BEVA开始,然后是5种二线治疗(sorafenib [SORA]、lenvatinib [LENVA]、regorafenib、cabozan- tinib和ramucirumab)的序列进行比较。从随机对照试验(RCT)中得出状态转换的概率(初始治疗、癌症进展和死亡)。获得年生存(LYG)是主要结果。计算严重不良事件(SAEs)(≥3级)发生率。
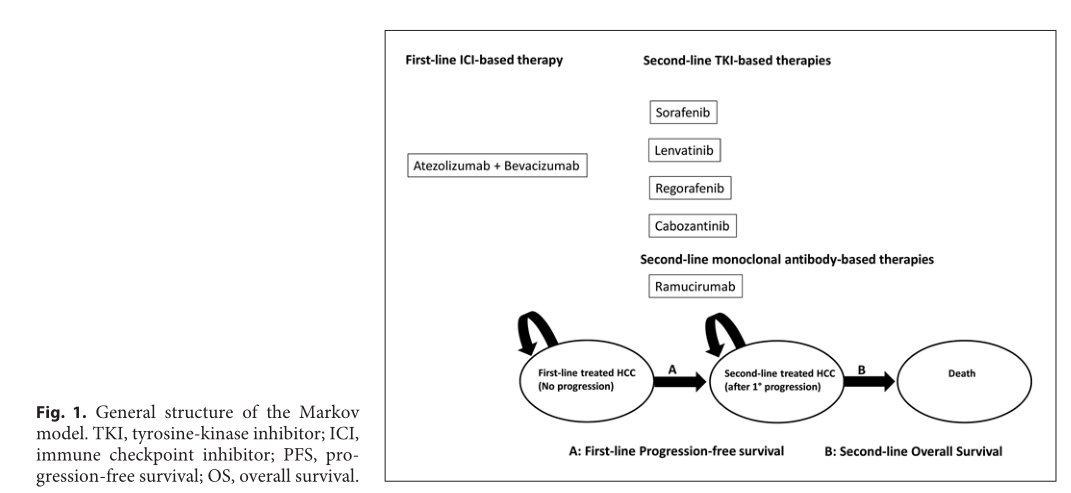
研究流程
一线ATEZO +BEVA治疗进展后,后续二线Lenvatinib治疗时中位OS为24个月(23–25),LYG为0.50年,SAEs %为67.8 %(66.3–69.3);2018年后Sorafenib治疗时中位OS为23个月(22–24),LYG为0.42年,SAEs %为63.0% (61.5–64.6);cabozantinib 治疗时中位OS为20个月(19–21),LYG为0.17,SAEs %为69.9% (68.5–71.4);regorafenib治疗时中位OS为20个月(19–21) ,LYG为0.17,SAEs %为70.0% (68.6–71.5);2018年前Sorafenib治疗时中位OS为20个月(19–21) ,LYG为0.17,SAEs %为68.8% (67.3–70.3);Ramucirumab 治疗时中位OS为18个月 (17–19),SAEs %为65.6% (64.1-67.1)。
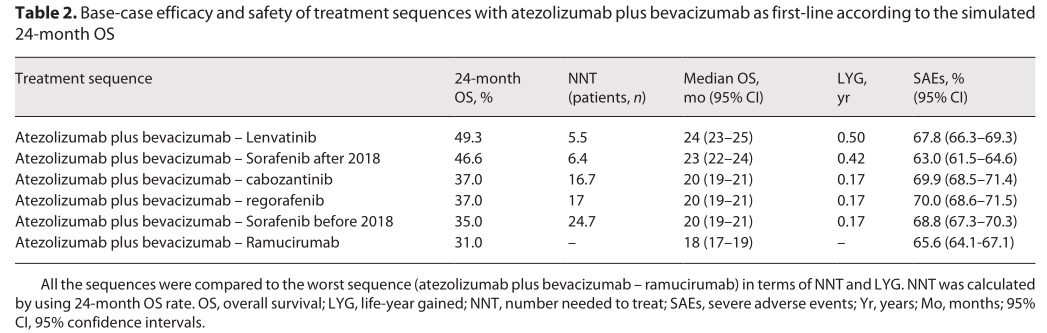
疗效、安全性对比
一线ATEZO +BEVA治疗进展后,后续二线Lenvatinib,2018年后Sorafenib,cabozantinib,regorafenib,2018年前Sorafenib和Ramucirumab治疗的24个月OS率分别为49.3%,46.6%,37.0%,37.0%,35.0%和31.0%。
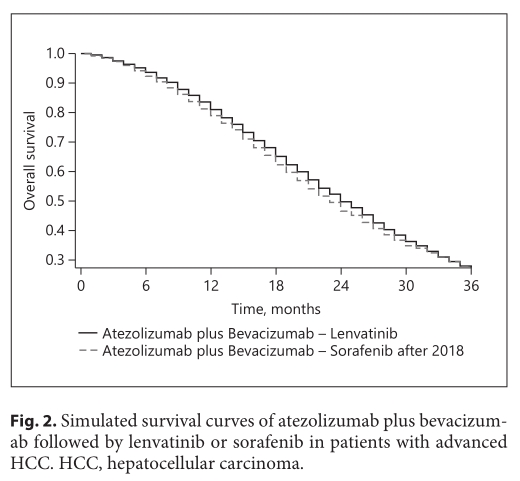
二线Lenvatinib,2018年后Sorafenib生存比较
综上,研究表明,atezolizumab (ATEZO) + bevacizumab (BEVA)一线治疗晚期HCC进展后,二线Lenvatinib或Sorafenib可能是最佳选择。需要后期随机对照临床研究去证实。
原始出处:
Giuseppe Cabibbo, Maria Reig, Ciro Celsa, et al. First-Line Immune Checkpoint Inhibitor-Based Sequential Therapies for Advanced Hepatocellular Carcinoma: Rationale for Future Trials.Liver Cancer. DOI: 10.1159/000520278. Published online: November 23, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#mAb#
53
#治疗选择#
61
#晚期HCC#
51
#HCC#
37
#二线治疗#
53
#Bevacizumab#
55
6
68