Radiology:稳定型冠脉疾病T1MRI高信号是斑块内出血而非脂质成分
2022-01-01 影像小生 MedSci原创
冠状动脉粥样硬化的T1加权平扫提供了血脂评估之外的更多关于斑块易损性的信息。
T1加权MRI平扫冠状动脉高信号斑块(HIPs)与较差的临床结果相关。在颈动脉中,斑块内出血(IPH)被认为是高信号的主要来源。然而,在MRI中冠状动脉HIPs的确切病理生理性质尚未确定。在稳定型冠状动脉疾病中,近期IPH的血脂和高铁血红蛋白T1值较短,两者都有可能产生高T1加权MRI信号。另一个复杂性是IPH通常存在于富含脂质斑块(LRP)中。
Shunya Sato等通过比较CATCH MRI扫描和近红外光谱(NIRS)血管内超声(IVUS)图像,确定T1加权图像上HIPs的主要底物是斑块内出血(IPH)还是脂质。该研究结果发表在Radiology杂志。
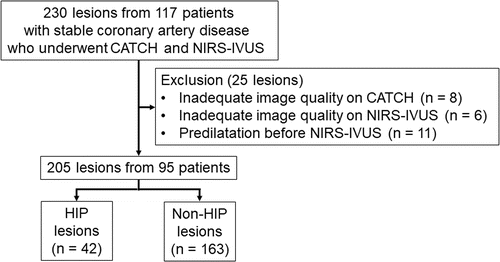
该研究回顾性地纳入了2019年12月至2021年2月在两个中心进行NIRS IVUS前进行CATCH MRI检查的连续患者。
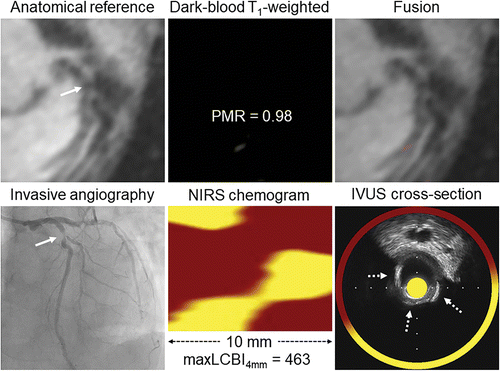
在MRI上,HIP被定义为斑块与心肌信号强度比至少为1.4。在IVUS(报告代表IPH)有回声带的存在被记录。采用近红外光谱法测定动脉粥样硬化斑块的脂质成分。脂核负担指数(LCBI)是感兴趣区域内脂核斑块概率大于0.6的像素的比例。将任何4 mm长的节段(maxLCBI4 mm)中LCBI最大值大于400的斑块定义为富含脂质。采用多变量分析来评估NIRS IVUS衍生的与HIPs相关的参数。

共分析了95名患者的205个斑块(中位年龄74岁;四分位间距[IQR], 67-78岁;75名男性)。MRI的HIPs (n = 42)主要与IVUS的无回声区 (分别为79% [33 / 42]vs 8.0% [13 / 163];P<0.001)和NIRS中较非HIPs高的maxLCBI4mm (477 [IQR, 258 738] vs 232 [IQR, 59 422];P<0.001)相关。

斑块-心肌信号强度比(PMR)和最大脂质核心负荷指数(maxLCBI4 mm)的散点图
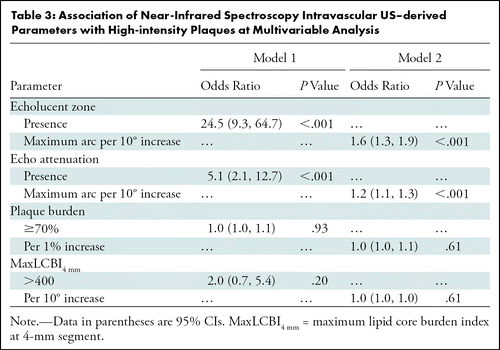
在多变量模型中,HIPs与无回声区独立相关(优势比,24.5;95%可信区间:9.3,64.7;P<0.001),但与富含脂质斑块无关(优势比,2.0;95%可信区间:0.7,5.4;P =0.20)。
在稳定型冠状动脉疾病中,T1加权MRI高信号斑块的主要底物是斑块内出血,而不是脂质。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#高信号#
83
#稳定型#
106
#斑块#
84
#斑块内出血#
112
#冠脉疾病#
84