JACC:溶栓治疗对斑块浸润引发的STEMI效果更佳
2014-01-25 清热解毒2号 dxy
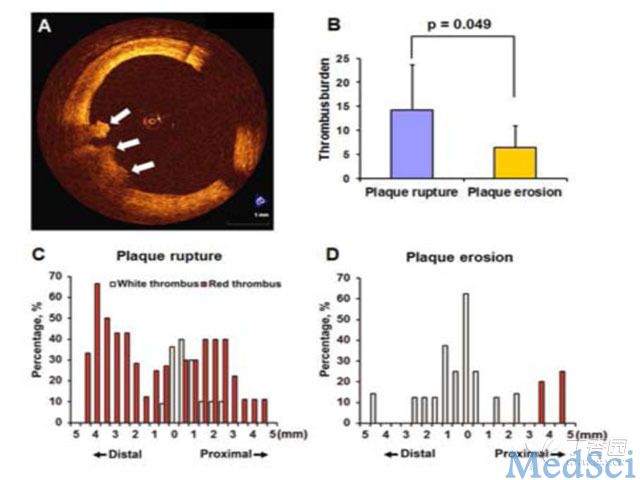
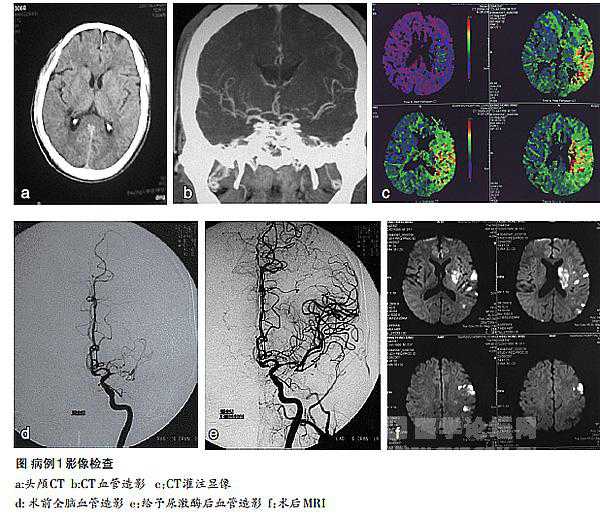
斑块浸润和斑块破裂都可导致血栓形成。斑块破裂时,坏死核心暴露于血液循环,成为血栓形成的主要诱因。而在斑块浸润中,蛋白多糖和平滑肌细胞被认为是血栓形成的主要刺激因素(图A)。由此可推测,溶栓治疗对斑块浸润引发的血栓比斑块破裂导致的血栓有更好的治疗效果。为此哈尔滨医科大学附属第二医院胡思宁等进行了一项研究,旨在比较斑块浸润与斑块破裂引发的STEMI在溶栓治疗成功再灌注后残余血栓的负荷、分布及特点。研究
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
51
#ACC#
63
#斑块#
74
#溶栓治疗#
70
#STEM#
61