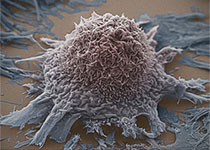
CELL HOST MICROBE:细菌为何引起结肠癌
2018-02-04 海北 MedSci原创
已有的研究显示,致癌细菌有可能具有启动和/或促进结肠癌的能力,该现象部分是通过免疫机制来作用,但是至今为止,我们对此还不完全了解。
已有的研究显示,致癌细菌有可能具有启动和/或促进结肠癌的能力,该现象部分是通过免疫机制来作用,但是至今为止,我们对此还不完全了解。
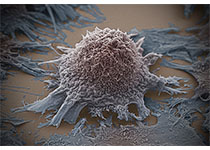
近日,来自霍普金斯大学医学院的研究人员利用一种微生物诱导结肠肿瘤发生的小鼠模型发现,脆弱拟杆菌毒素(BFT)可以触发一种致癌的,多步骤的炎症级联反应,这个过程需要在结肠上皮细胞(CECs)中表达的IL-17R,NF-κB和Stat3信号的参与 。
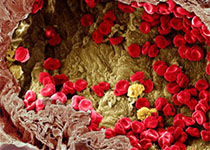
尽管是必要的,但CEC中的Stat3激活本身还是不足以触发ETBF结肠肿瘤发生。值得注意的是,CEC中IL-17依赖性的NF-κB活化能够诱导C-X-C趋化因子(包括CXCL1)的近端至远端粘膜梯度,其能够介导表达CXCR2的多形核未成熟骨髓细胞的募集,并促进ETBF介导的远端结肠肿瘤的发生。
因此,BFT从CEC诱导致癌性信号传导至粘膜Th17应答,导致远端结肠CECs中发生选择性的NF-κB活化,其共同触发髓细胞依赖性远端结肠肿瘤的发生。
原始出处:
Liam Chung et al. Bacteroides fragilis Toxin Coordinates a Pro-carcinogenic Inflammatory Cascade via Targeting of Colonic Epithelial Cells. Cell Host & Microbe, 2018; DOI: 10.1016/j.chom.2018.01.007
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
59
#Cell#
82
#CRO#
52
#Micro#
94
.学习了提高了
90
谢谢分享学习了
84
学习谢谢分享
85