5月31日,第14届东方心脏病学会议(OCC2020)遇见新未来—抗栓策略前沿论坛上,来自复旦大学附属中山医院心内科的钱菊英教授结合最新的循证医学证据跟自身多年临床经验全面介绍了冠心病抗栓方案。
冠心病的分类,病理机制及远期心血管风险
冠心病根据发病特点和治疗原则,主要分为慢性冠脉综合征(CCS)和急性冠脉综合征(ACS),因冠状动脉发生粥样硬化病变而严重阻塞或闭塞,导致心肌缺血、缺氧或坏死而引起,归属为缺血性心脏病。冠心病患者预后主要决定因素为冠脉病变累及心肌供血的范围和心功能。远期心血管风险包括急性心肌梗死、冠心病猝死以及缺血性脑卒中等。抗栓治疗始终是冠心病一/二级预防的重要方面,在二级预防中作用更显著。
冠心病二级预防抗栓方案
无论是慢性冠脉综合征,还是急性冠脉综合征,均必须进行抗血小板治疗,这在减少动脉血栓事件方面具有明确的获益证据。阿司匹林基本上是所有抗栓治疗方案的基线抗血小板用药。冠心病合并其他心血管事件时,需要联合用药,改善预后。联合用药方案如下:窦性心律合并冠心病时,在阿司匹林基础上,联合应用另一种抗血小板药物,主要是P2Y12受体抑制剂;CCS患者主要联用氯吡格雷;ACS患者首选作用更强的P2Y12受体抑制剂,如替格瑞洛/普拉格雷/氯吡格雷。用药种类、用药时间主要根据患者缺血风险和出血风险确认,制定个体化的策略。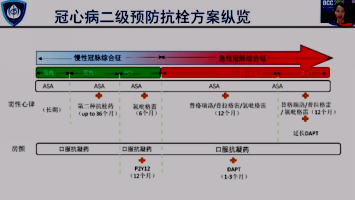
CCS患者出现高危缺血风险,如心肌梗死、合并糖尿病、多肢循环病变、慢性肾功能不全或者出现周围循环疾病时,可以联用P2Y12受体抑制剂,治疗延长到36个月,以减少缺血事件的发生。ACS基本都采取双联抗血小板治疗12个月,但部分出血高风险患者或接受介入治疗的患者,应缩短疗程。房颤合并冠心病患者,抗血小板与抗凝治疗要同时进行,以减少血栓栓塞事件。
抗栓方案纵览
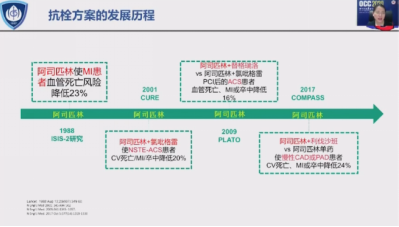
1988年ISIS-2研究分为阿司匹林组和安慰剂组,对17187例24小时内疑似心肌梗死患者平均随访15个月。结果显示阿司匹林使MI患者死亡风险降低23%,奠定了阿司匹林抗血小板治疗基线药物的地位。
2001年CURE研究结果表明双抗治疗(阿司匹林联用氯吡格雷)较阿司匹林使非ST段抬高型急性冠脉综合征(NSTE-ACS)患者急性期(24h)和长期(12m)的缺血事件风险分别降低34%和20%,且不增加致死性缺血风险。开启了ACS双抗治疗时代,尤其为抗栓治疗12个月提供循证医学证据。
针对氯吡格雷起效慢、需要药物代谢后发挥作用的不足。2009年PLATO研究比较了阿司匹林联用替格瑞洛和阿司匹林联用氯吡格雷的疗效。结果表明前者相比于后者使PCI后的ACS患者心血管事件风险降低了16%。将心血管风险风高的ACS患者的抗栓治疗升级为阿司匹林联用替格瑞洛。
2017年COMPASS研究,患者分别接受阿司匹林联用利伐沙班、利伐沙班或阿司匹林治疗。阿司匹林联用利伐沙班相比阿司匹林单药使慢性CAD或PAD患者CV死亡、MI或卒中风险降低24%。该方案比较适合高缺血风险、无高出血风险的CCS患者。COMPASS研究开启了CCS患者抗血小板+抗凝双通道抗栓新时代。
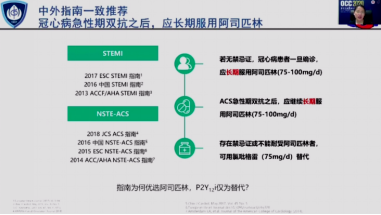
阿司匹林在抗栓治疗的地位众所周知,但是因为阿司匹林具有引起增加消化道出血的风险,在冠心病一级预防中也出现了质疑的声音。柳叶刀杂志5月9日发表的大样本系统评价与Meta分析,是全球首个在二级预防领域研究纳入替格瑞洛,并与阿司匹林全面比较的系统评价。全面综合地评估了P2Y12抑制剂(氯吡格雷、替格瑞洛)和阿司匹林两类单药在ASCVD二级预防的疗效差异。结果显示阿司匹林和P2Y12抑制剂方案治疗的患者在全因死亡、血管死亡、卒中风险均无显著差异。
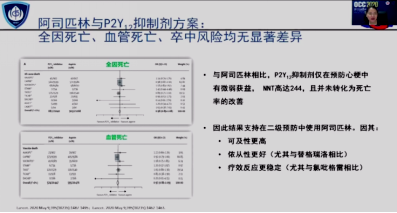
接受P2Y12抑制剂治疗的患者在疗效上上并没有优于阿司匹林,反而在任何出血发生风险方面,阿司匹林结果反而更优,特别是阿司匹林对比替格瑞洛的研究中,阿司匹林出血事件发生率更低。因阿司匹林可及性更好,依从性更好,疗效反应更稳定。综合这些因素考量,阿司匹林作为心血管疾病二级预防的基石地位是不可替代的。
当冠心病合并房颤:抗血小板与抗凝治疗怎样兼顾?
房颤和冠心病共享很多高危因素:高龄,高血压,糖尿病等。冠心病引起心功能不全也会增加房颤的发生率,ACS引发的缺血性心功能不全也能引起新发的房颤。GARFIELD研究表明我国32.4%的房颤患者合并有冠心病,2019AHA/ACC/HRS房颤指南表明ACS患者中合并房颤比列达10-21%。对冠心病合并房颤的患者,同时进行抗血小板与抗凝治疗时,需要思考如下问题:(1)抗血小板药物双联治疗持续时间。(2)既有抗血小板又有抗凝适应症时,如何确定三联用法。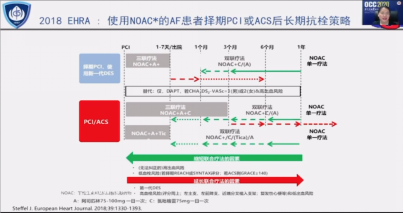
2018年EHRA指南指出:针对有新型口服抗凝药(NOAC)适应症的房颤患者进行择期PCI或ACS后长期抗栓,要评估患者出血和血栓栓塞的风险,来抉择缩短或延长联合治疗时间。对于具有抗凝适应症的患者,NOAC相比华法林可以减少监测、相对更稳定、药物相互作用更少,在保证疗效的情况下出血风险更低;对于择期PCI患者,使用新一代DES,三联治疗的时间可以尽可能缩短,在出院时就改用两联治疗即NOAC+抗血小板药物(首选氯吡格雷)治疗,出院一年后稳定的病人可以单用口服抗凝药。针对PCI/ACS的患者,若无出血高风险,有缺血或血栓的高风险,应该延长NOAC+双联抗血小板药物联合治疗(三联治疗)的时间至三个月,然后改为两联治疗即NOAC+抗血小板药物(首选氯吡格雷)。若有高出血风险,三联治疗应缩短到住院期间。
循证医学的证据表明,在房颤合并ACS/PCI术后一年内,NOAC+氯吡格雷双联抗栓治疗,相比于华法林+双联抗血小板治疗,降低出血事件的同时不增加缺血事件。在超过一年的稳定型病人当中,单用利伐沙班与抗血小板治疗相比,缺血事件发生率相当。
DAPT方案的现状与探索
在冠心病抗栓治疗领域,DAPT的疗程问题一直存在争议。2017年ESC/EACTS DAPT指南更新,治疗策略为:SCAD患者用阿司匹林+氯吡格雷,DAPT时长至少6个月;对ACS患者,用阿司匹林+普格瑞洛/普拉格雷/氯吡格雷治疗至少12个月。关于治疗时间也有延长和缩短的因素(如下图),缩短双抗时长的目的在于不增加缺血风险的同时降低患者的出血风险;延长双抗治疗目的是在进一步降低缺血风险的同时,出血风险不增加或增加在可接受范围内。
特殊情况下DAPT方案的探索,要综合判断缺血出血风险,决定时长,使净获益最大化。高缺血风险患者要延长DAPT时程;高出血风险患者要缩短DAPT时程。
总结
制定抗栓治疗方案应结合患者冠心病类型(慢性冠脉综合征还是急性冠脉综合征)、缺血和出血事件风险、临床特点、、是否曾进行血运重建、是否有联合抗凝的适应证来制定个体化方案。把握缺血和出血风险之间的平衡显得尤为重要,临床上应特别关注高缺血风险合并出血风险的患者。
最后钱教授总结道:(1)抗栓治疗始终是冠心病一/二级预防的重要方面。(2)冠心病二级预防的抗栓方案,以阿司匹林为基石的抗血小板药物和新型抗凝药的联合应用不断发展。(3)DAPT方案不断细化,临床上实行个体化评估治疗,以实现缺血与出血风险的平衡。讲座结束后,钱菊英教授跟与会的其他专家讨论到:冠心病患者病情各不相同,制定个体化方案非常重要。出血风险的评估是一个动态的过程,需要临床医生具有更敏捷的临床思维。随着介入技术的发展,双抗方案也会相应的进行改变。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










涨姿势了✌️
64
请问有相关指南吗
67
不错,值得学习
89
#钱菊英#
64
#OCC#
56
#OCC 2020#
56