HUMAN BRAIN MAPPING:重度抑郁症患者神经质、快感缺乏等症状与特定白质连接有关
2021-07-25 MedSci原创 MedSci原创
该研究发现为MDD的状态和特质变量对大脑连接和认知的差异影响提供了证据。多变量方法显示了解释MDD内异质性的可行性,并将其追踪到特定的脑回路,从而增加了对生物学水平上异质性的更好理解。
重性抑郁障碍(MDD)的异常脑结构连接性已被反复报道,然而以往的许多研究缺乏将MDD的不同特征与多变量建模方法中的结构连接相结合。
Igor Nenadić等检验了白质束完整性与快感减退、焦虑、神经质和不同区域束认知控制相关的假设。研究结果发表在HUMAN BRAIN MAPPING杂志。
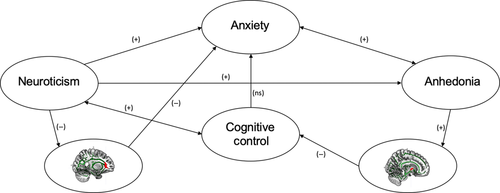
首先测试了一个整合了快感、神经质、焦虑和认知控制的结构方程。然后分析了白质连接与临床变量的关系,最后利用SEM将其整合到一个可测试的多变量模型中。更准确地说,基于上述几项关于脑成像和快感缺失的研究,预计快感缺失主要与情绪调节相关的脑结构畸变有关,例如ATR、UF。由于先前对DTI和负相关情绪的研究表明UF参与了这一过程,该研究期望在这一过程中发现与神经质以及焦虑的关联。将认知控制分别建模为执行功能或抑制能力,基于先前的研究发现,这些认知控制不仅在MDD中受损,而且与MDD的特定风险因素有关。
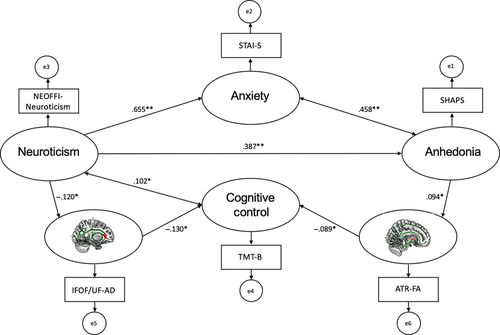
该研究招募了595例MDD患者,采用结构方程模型(SEM)在一个综合模型中检验了无快感、焦虑、神经质和认知控制之间的相互关系。然后,分别分析了扩散张量成像(DTI)连接测量与这些临床变量的关系,最后将脑连接关联、临床/认知变量整合到一个多变量SEM中。
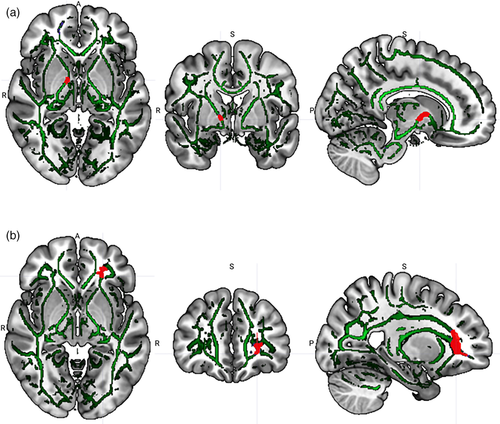
首先确认了临床/认知结构方程模型。DTI分析(FWE校正)显示,无食欲与右前丘脑放射(ATR)和小钳/胼胝体的部分各向异性(FA)呈正相关,而神经质与左钩束(UF)和额枕下束(IFOF)的轴向扩散率(AD)呈负相关。扩展SEM证实了ATR-FA与快感缺乏的关系,UF/IFOF AD与神经质影响认知控制的关系。
该研究提出了多元关系模型。提出了多元关系模型。矩形表示观测变量,椭圆表示误差调整后的潜在变量。(+)和(-)表示在p<.05时关系达到显著性的假设方向。单头箭头代表回归,双头箭头代表相关。与脑成像数据的关系:神经质-IFOF/UF-AD簇-焦虑;快感缺乏-ATR-FA簇-认知控制。
该研究发现通过指定MDD表型变量的共享连接网络,推进了目前对MDD白质微结构的理解。在DTI分析中发现的大脑结构相关显示了两种自主连接路径,一种代表人格特质对大脑结构的影响,另一种代表MDD样本中主要症状对大脑结构的影响。然而,两者对认知控制的影响是相互独立的。这表明MDD中的“断开综合征”比先前研究MDD中大脑连接网络时最初提出的更为可靠。因此,与以往的MDD脑连接研究相比,该研究为MDD特征在脑结构水平上的相互关系提供了有意义的见解。此外,研究结果还提供了一种连接组方法来分离症状群和神经基础,最终可以服务于个性化治疗计划。
原文出处
Brain structural connectivity, anhedonia, and phenotypes of major depressive disorder: A structural equation model approach. https://doi.org/10.1002/hbm.25600
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#白质#
71
#human#
56
#抑郁症患者#
60
#mapping#
61
受益匪浅
0