Research:浙大闵军霞/王福俤团队提出食管鳞癌治疗全新策略,靶向LSD1-G9a-ER应激通路
2022-06-10 “生物世界”公众号 “生物世界”公众号
在我国,绝大部分(90%)食管癌患者属于食管鳞状细胞癌(ESCC),而患者在诊断时往往已处于晚期,5年生存率仅为20%左右。因此,发现食管鳞状细胞癌的治疗新靶点并开发相应治疗药物显得尤为迫切。
据世界卫生组织国际癌症研究署(IARC)发布的2020年全球癌症负担数据,食管癌是世界年新增人数第8,年死亡人数第6的恶性肿瘤。而且,食管癌在中国尤为突出,全球每年新增和死亡的食管癌,均有超过一半在中国。
在我国,绝大部分(90%)食管癌患者属于食管鳞状细胞癌(ESCC),而患者在诊断时往往已处于晚期,5年生存率仅为20%左右。因此,发现食管鳞状细胞癌的治疗新靶点并开发相应治疗药物显得尤为迫切。
近日,浙江大学医学院闵军霞教授/王福俤教授团队在国际著名学术期刊 Research 上发表了题为:Targeting the LSD1-G9a-ER Stress Pathway as a Novel Therapeutic Strategy for Esophageal Squamous Cell Carcinoma 的研究长文。
该研究发现,同时抑制组蛋白去甲基化酶 LSD1 和组蛋白甲基转移酶 G9a 能够显着协同抑制食管鳞状细胞癌(ESCC),而靶向内质网应激(ER-stress)通路能够进一步增强对食管鳞状细胞癌的抑制效果。
这些发现为靶向 LSD1、G9a 和 ER-stress 来治疗食管鳞状细胞癌的临床转化研究提供了新策略。
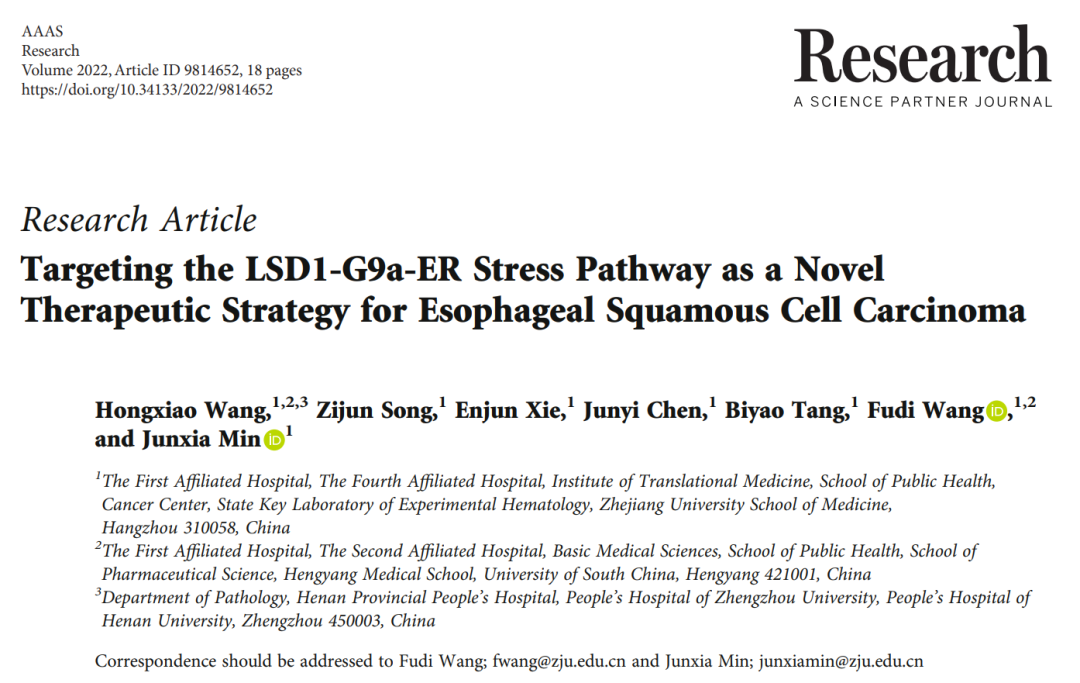
该研究通过运用不同类型肿瘤细胞系对39种表观遗传小分子药物库进行功能筛选,发现 LSD1 的抑制剂 SP2509 及 G9a 的抑制剂 BIX01294 显着抑制多种肿瘤细胞生长。
进一步功能验证研究发现:同时抑制组蛋白去甲基化酶 LSD1 和组蛋白甲基转移酶 G9a 显着协同抑制食管鳞状细胞癌(ESCC)生长活力及克隆形成能力(CI50<1:协同致死效应),但对肝癌(HepG2、Huh-7)、胃癌(AGS)、急性T细胞白血病(Jukat-1)、肺癌(A549)、人纤维肉瘤(HT1080)等其它类型肿瘤细胞系并无明显影响。
为了进一步确认 ESCC 的生存活力依赖于 LSD1 和 G9a,研究团队通过四环素诱导的 shRNA 基因敲降实验发现:shLSD1 及 shG9a 能够显着抑制 ESCC 细胞活力和人源食管鳞癌肿瘤细胞的小鼠移植瘤生长,提示同时靶向抑制 LSD1 和 G9a 可成为食管癌治疗新策略。
进一步食管鳞癌荷瘤小鼠结果证实:联合 LSD1 和 G9a 的小分子抑制剂能够通过抑制 ESCC 增殖及促进其凋亡显着抑制小鼠 ESCC 肿瘤生长,该成果为临床转化提供重要依据。
靶向LSD1和G9a诱导食管鳞癌细胞协同致死并抑制体内成瘤
LSD1(Lysine specific demethylase 1)是第一个被发现的组蛋白去甲基化酶,依赖黄素腺嘌呤二核苷酸(FAD)特异性脱去组蛋白H3第4位赖氨酸(H3K4)和第9位赖氨酸(H3K9)上的单甲基和二甲基。既可以与 CoREST 或 NuRD 互作发挥转录抑制作用,也能与雄激素受体(AR)互作发挥转录激活功能。
G9a 做为组蛋白甲基转移酶,主要催化组蛋白H3第9位赖氨酸(H3K9)的单甲基化、二甲基化,在转录、信号转导、细胞增殖和分化中发挥重要作用。尽管已有文献报道 LSD1 或 G9a 在食管癌发生发展中可能发挥重要作用,但两者是否存在协同效应及其分子机制尚待深入研究。
为了探究 LSD1 和 G9a 与食管癌患者的临床相关性,研究者通过 TCGA 数据库分析发现食管癌组织中 LSD1 及 G9a 基因在转录组水平均显着高于正常组织;随后,通过114例中国食管鳞癌患者的组织芯片的免疫组化结果分析发现:
1)食管鳞癌组织中 LSD1 及 G9a 蛋白表达水平明显高于正常对照组织;
2)LSD1 与患者年龄及原发肿瘤分期(T stage)显着相关;
3)G9a 与患者的肿瘤分级(grade)及增殖指数(Ki67)显着相关;
4)LSD1 和 G9a 同时高表达的食管鳞癌患者的总生存期最短。
功能研究显示 ESCC 中同时过表达 LSD1 和 G9a 显着促进 ESCC 细胞生长。这些临床及体外研究均提示 LSD1 和 G9a 是食管鳞癌治疗潜在新靶点。

LSD1和G9a的高表达与食管鳞癌患者不良预后的相关性
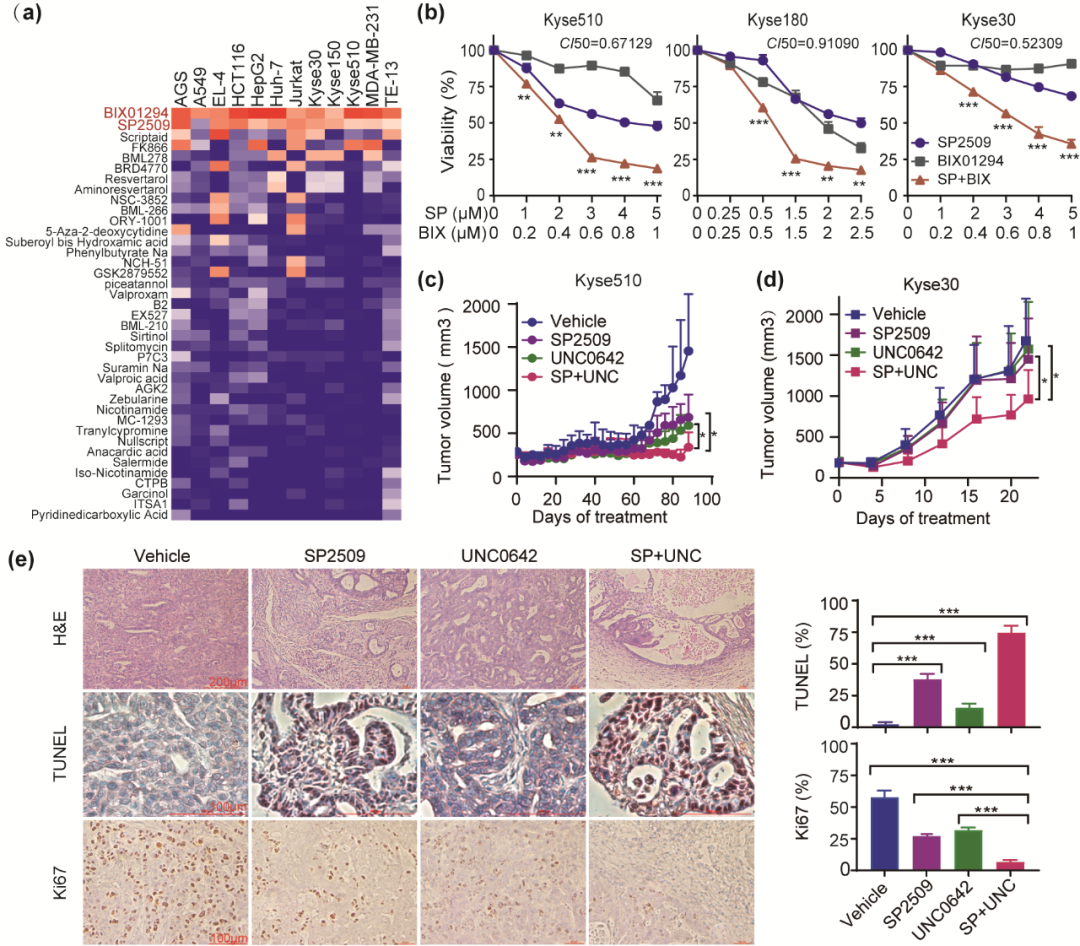
为了探索机制,通过转录组测序整合分析及功能验证研究发现:抑制 LSD1 和 G9a 主要通过诱导细胞周期阻滞和细胞凋亡促进食管鳞癌细胞死亡;同时,显着下调内质网应激(ER-stress)相关基因的表达,如 PERK、ATF4、Chop、eIF2a、ATF6、IRE1a。
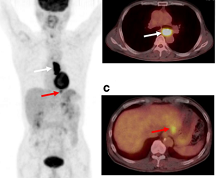
此外,研究者发现靶向 ER-stress 不仅使 ESCC 对单独的 LSD1 或 G9a 抑制剂更加敏感,而且显着促进同时抑制 LSD1 和 G9a 的食管鳞癌细胞的死亡并进一步抑制小鼠 ESCC 肿瘤生长,这些结果为靶向 LSD1、G9a 和 ER-stress 治疗食管鳞癌的临床转化研究提供了新策略。

靶向ER-stress促进食管鳞癌细胞对LSD1和G9a抑制剂的敏感性
成果总结:
1)通过表观遗传分子库筛选、功能验证,揭示 LSD1 和 G9a 在食管鳞癌发生发展中具有重要作用。
2)食管癌患者组织芯片及 TCGA 临床数据库分析,表明 LSD1 和 G9a 表达与食管鳞癌患者的疾病进展及总生存期显着相关。
3)通过转录组分析及体内、体外功能及机制研究,揭示靶向 LSD1、G9a 和 ER-Stress 三种治疗策略叠加可显着抑制 ESCC 细胞生长及成瘤能力,起到良好的肿瘤治疗作用。
4)本成果为食管鳞癌治疗提供了潜在新靶点及治疗崭新策略,具有重要的临床转化意义。
论文第一作者为博士研究生王红晓;通讯作者为闵军霞教授和王福俤教授。博士研究生宋秭君、谢恩军和汤碧瑶为参与作者。浙江大学医学院/转化医学研究院/公共卫生学院,附属第一医院和附属第四医院为作者贡献单位。论文成果得到国家自然科学基金委及国家科技部项目资助。
原始出处:
Hongxiao Wang, et al. Targeting the LSD1-G9a-ER Stress Pathway as a Novel Therapeutic Strategy for Esophageal Squamous Cell Carcinoma. Research, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#闵军霞#/#王福俤#团队提出#食管鳞癌#治疗全新策略,#铁死亡#
96
#食管#
58
#LSD1#
46
#应激#
60
#新策略#
75
#鳞癌#
52
#浙大#
61
#ER应激#
59
#Research#
48