在英国,每年有超过12万人经历脚踝骨折。这类骨折是一种严重的创伤负担,由于老年活动者的数量不断增加,预计到2030年踝关节骨折将增加三倍。通常情况下,骨折后踝关节需要用石膏固定数周,这样可以使骨头愈合,但也会导致关节僵硬和肌肉无力。另一种选择是一个可移动的支架。使用可移动支架可以防止僵硬固定的后果,并有助于加速恢复。这两种方法在英国都很常用。

一项Cochrane综述总结道,功能性支具虽然可以减少活动受限和疼痛,改善踝关节运动。然而,这些潜在的优势需要与不良事件发生率的增加进行综合考量。目前尚无高质量的证据支持踝关节骨折后早期活动的有效性或安全性。
鉴于此,有研究小组评估了使用石膏固定与使用可移动支架治疗踝关节骨折的成人患者的功能、生活质量、资源使用和并发症。该研究结果今日发表在BMJ期刊上。
本研究为一项多中心随机对照试验,英国国民医疗服务体系的20个创伤病房加入研究。纳入669名年龄在18岁以上的适合使用石膏固定的急性踝关节骨折患者:334名随机使用石膏固定,335名随机使用可移动支架。主要结果是16周时Olerud Molander踝关节评分,根据治疗意图进行分析。次要结果是曼彻斯特-牛津足部问卷、残疾评分指数、生活质量以及6周、10周和16周的并发症。
研究数据显示,参与者的平均年龄为46岁(标准差17岁),381名(57%)为女性。502名(75%)参与者完成了研究。16周时,石膏组和可拆卸支架组的Olerud Molander踝关节评分无统计学差异(Favors支架:1.8,95%置信区间2.0至5.6)。在其他时间点的Olerud Molander踝关节评分、次要未调整分析、插补分析或按方案分析中未发现临床显著性差异。95%置信区间的上限有效地排除了一种干预优于另一种干预的可能性。
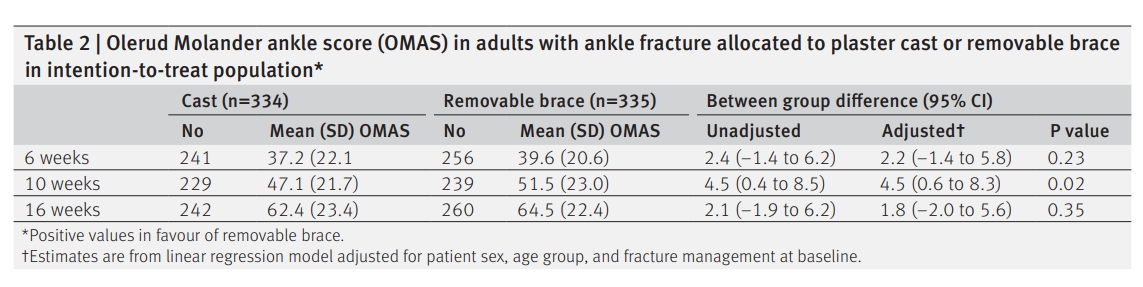
Olerud Molander踝关节评分(OMAS)在意向治疗人群中对踝关节骨折采用石膏或可拆卸支架
在次要时间点Olerud-Molander踝关节评分或ManchesterOxford足部问卷的次要结果测量、残疾分级指数、生活质量和并发症方面未发现临床相关差异。研究者发现两种干预措施在严重并发症的安全性方面没有统计学上的显著差异。可拆卸支架具组并发症发生率较高,尤其是伤口破裂(7v15)、伤口感染(10v19)和需要进一步手术(4v8)的风险。然而,该研究无法检测这些次要结果的差异。
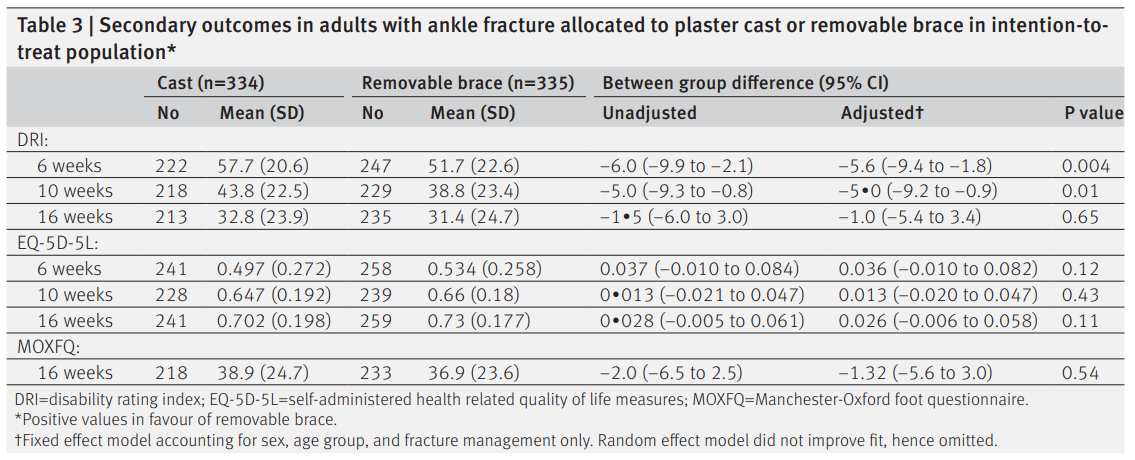
使用石膏或可拆卸支架治疗成人踝关节骨折的次要结果
总之,该试验为成人踝关节骨折的传统石膏固定和可移动支具之间没有统计学上的显著差异提供了有力的证据。未来的研究应考虑初始固定阶段后的后期康复的重要性。
参考文献:Use of cast immobilisation versus removable brace in adults with an ankle fracture: multicentre randomised controlled trial BMJ 2021; 374 doi: https://doi.org/10.1136/bmj.n1506 (Published 06 July 2021)Cite this as: BMJ 2021;374:n1506
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BMJ#
66
#踝关节骨折#
119
#踝关节#
70
学习了
96
学习学习
77