【一般资料】
患者,男,21岁
【主诉】
以“外伤后胸背部疼痛双下肢瘫痪1月余”为主诉入院。
【现病史】
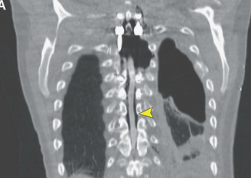
患者于1个月前溜冰时摔倒致伤,当时感胸背部疼痛,未做任何检查,在家休养,外敷膏药治疗,于2周前开始出现双下肢无力、行走不稳,在当地诊所输液治疗(用药不详),3d前双下肢无力症状加重、无法下地行走,于12h前出现大小便功能障碍,遂由家人急诊送至我院。胸椎CT提示“T3椎体形态改变、T3椎体骨质不连续”。
【既往史】
患者平素无发热、消瘦、盗汗等症状,家族无肿瘤病史,触摸全身浅表淋巴结未见肿大。
【体格检查】
T2~3棘突压叩痛阳性,双侧乳头连线以下平面感觉明显减退,部分感觉丧失;双下肢肌力0级,腹壁反射消失,双膝跟腱反射消失,肛门括约肌反射及提睾反射消失,双侧巴彬斯基征阳性。
【辅助检查】
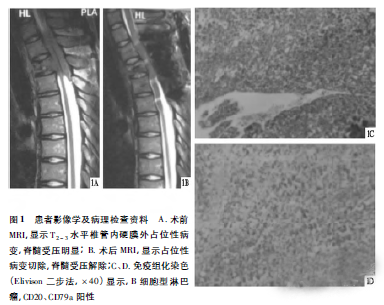
胸椎MRI(见图1A)显示:T3椎体楔形改变,其内可见长T1短T2信号,T2~3水平椎管内硬膜外可见一梭形高T1、T2信号,脊髓受压。实验室检查:肝功生化、红细胞沉降率、C-反应蛋白、血常规、凝血四项、结明实验均未见异常。
【初步诊断】
因患者有明确的外伤史,初步诊断为创伤性椎管内硬膜外血肿。
【治疗经过】
考虑病情进展较快,患者入院3d前双下肢已完全瘫痪,遂于入院第2天在全身麻醉下行胸椎管内血肿清除术。术中见平T2椎板中上缘至T3椎板下缘硬膜外有一2CM×1CM×1CM大小的灰白色软组织块,质软易碎,与周围组织粘连,彻底清除病灶。术后复查胸椎MRI,显示椎管内占位解除,脊髓减压彻底(见图1B)。但术后12d内患者的双下肢肌力、感觉均未见改善。术后病理(见图1C、D):椎管内硬膜外非霍奇金淋巴瘤(B细胞型),免疫组化显示肿瘤细胞:CD20、CD79a阳性,CD3、CD43、CD45RO、CK8/18、CD138阴性,Ki-67为80%。术后最终诊断:原发性椎管内硬膜外非霍奇金淋巴瘤。患者拒绝转肿瘤科治疗,术区伤口愈合后出院。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#硬膜外#
98
学习了.谢谢作者分享!
93
#硬膜外血肿#
75
#椎管内#
94
#椎管#
74
好好学习天天向上
106
谢谢分享.谢谢.学习了
129
学习
86
#血肿#
112