J Gastroenterology H: 无细胞浓缩腹水回输疗法 (CART) 对肝硬化腹水患者具有良好的治疗效果
2021-07-14 MedSci原创 MedSci原创
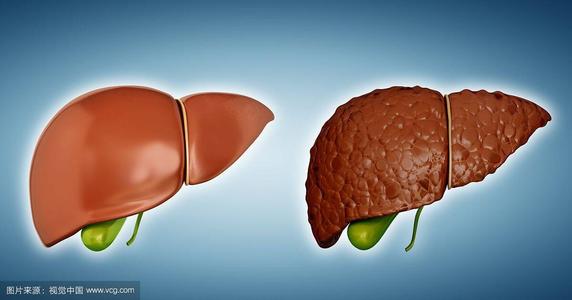
腹水是失代偿期肝硬化患者最常见的并发症之一。无细胞和浓缩腹水回输疗法(CART)已用于治疗肝硬化腹水。
腹水是失代偿期肝硬化患者最常见的并发症之一。无细胞和浓缩腹水回输疗法(CART)已用于治疗肝硬化腹水,但其安全性和有效性、CART 治疗不同病理背景的恶性肿瘤相关腹水的临床特征差异仍不清楚。因此,本项研究旨在对无细胞浓缩腹水回输疗法 (CART) 对肝硬化腹水的有效性进行相关研究。

本研究收集了22 个临床中心进行的 CART 前瞻性实验的受试者数据。分析了每个程序的状况、患者的治疗选择、实验室数据、患者临床表现状态、饮食摄入量和腹围。并比较了CART前后的临床参数,以及有或没有白蛋白输注以及包括肝硬化和恶性疾病在内的原发性疾病的差异。
研究结果显示在2014 年 1 月至 2015 年 1 月期间,所有研究机构共对肝硬化和恶性肿瘤患者进行了300多次CART手术。在肝硬化患者中,同时输注和不输注白蛋白组的血清白蛋白浓度显着增加(p=0.023),这些组之间的 CART 间隔没有显着差异(p=0.393)。CART 间隔在肝硬化和恶性肿瘤组之间没有显着差异(p = 0.334)。两组在 CART 后饮食摄入量均显着改善(p=0.043 和 <0.001)。
本项研究证实CART 在与失代偿期肝硬化相关的腹水患者中可以安全有效地进行,并在恶性肿瘤患者中提供了维持血浆胶体渗透压的潜在功效。
原始出处:
Tetsuya Ito. Et al. Safety and efficacy of cell-free and concentrated ascites reinfusion therapy (CART) against cirrhotic ascites in comparison with malignancy-related ascites. J Gastroenterology H.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GAS#
52
#Gastroenterol#
57
#治疗效果#
46
#AST#
62
#肝硬化腹水#
57
#ART#
52
#cART#
67
#Gastroenterology#
43
谢谢梅斯提供这么好的信息,学到很多
69
谢谢!最新的信息读起来就是收获大
73