Nat Med:白血病细胞家谱绘制成功!改写传统治疗方案!
2018-07-18 Zoe 转化医学网
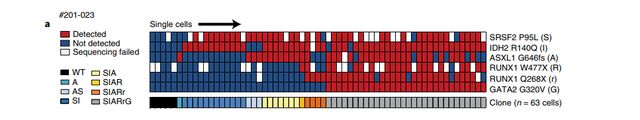
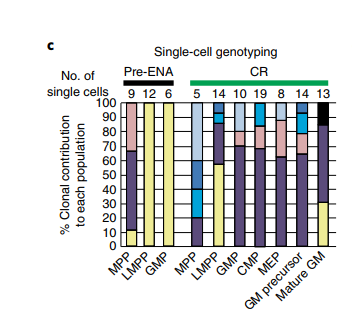
近日,Gustave Roussy 癌症研究所的研究人员首次绘制了急性髓性白血病(AML)癌细胞的细胞家谱,继而可以获悉这种血癌对新药enasidenib的反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
65
#治疗方案#
54
#细胞家谱#
51
#Med#
52
学习学习很好
121
学习了长知识
90